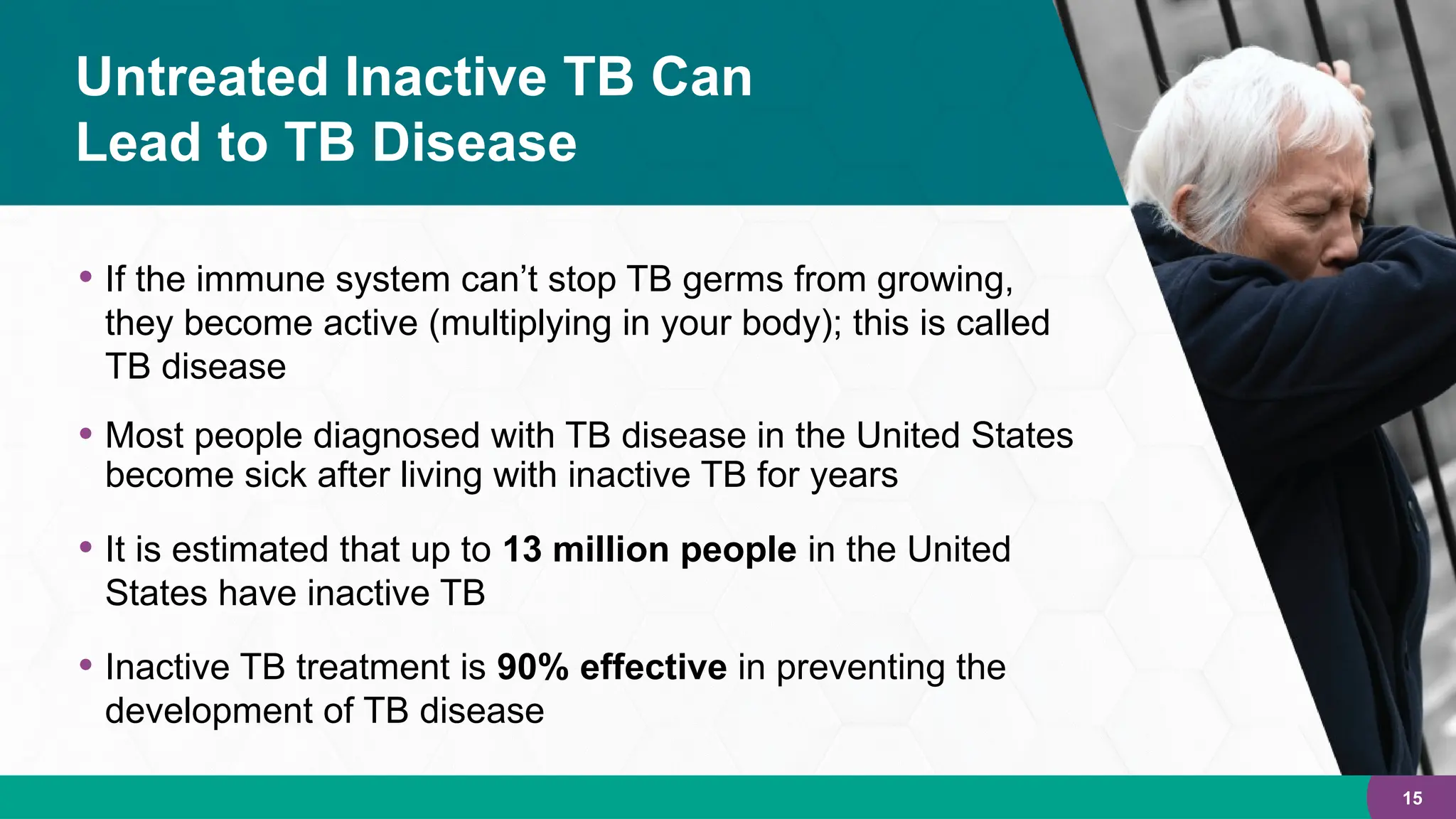
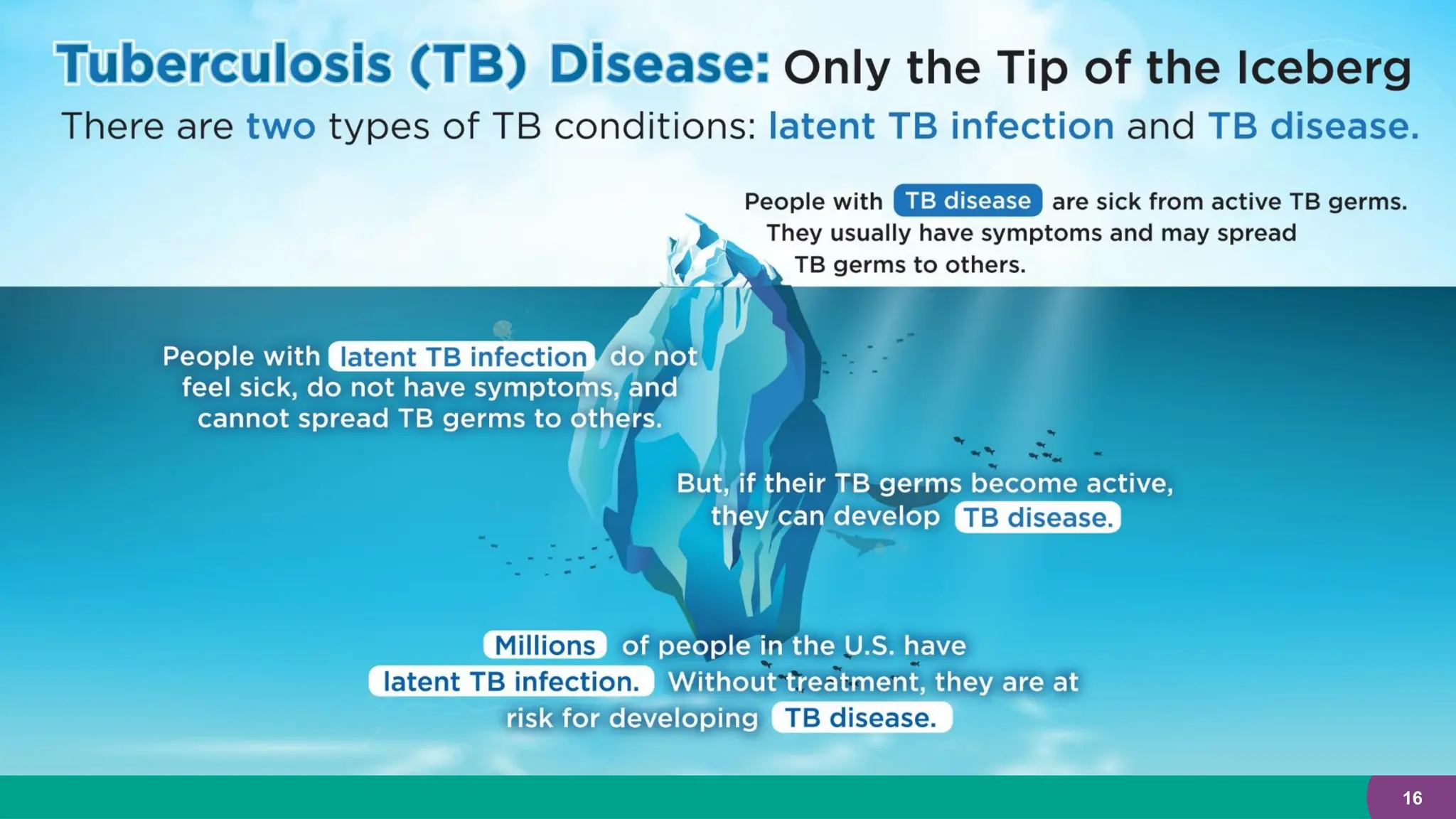
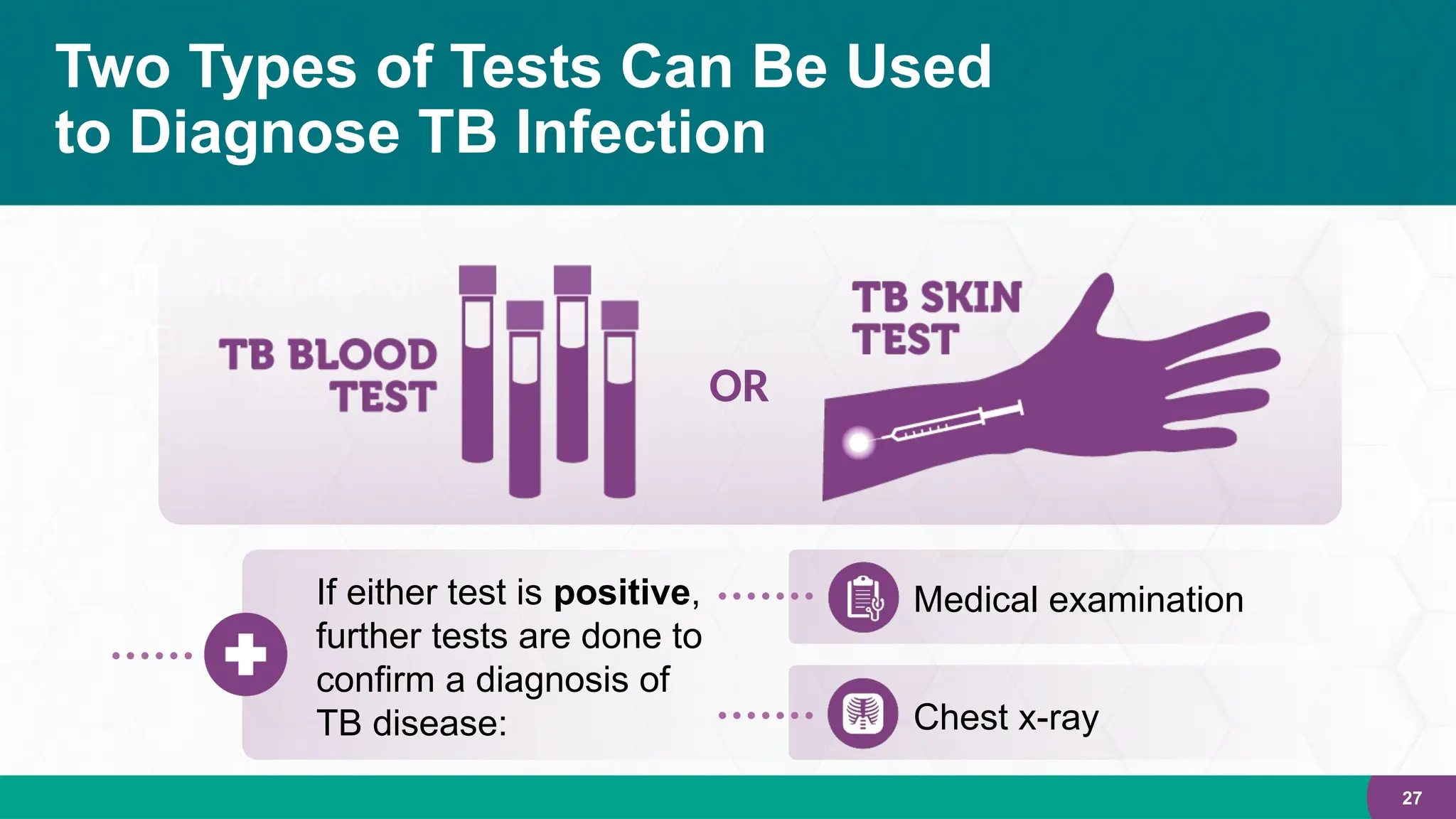
This document provides a comprehensive overview of tuberculosis (TB), covering its characteristics, transmission, types, symptoms, and treatment options. It highlights the continuing impact of TB as a significant global health issue, particularly in the United States, and discusses strategies for TB testing, management, and elimination. The document emphasizes the importance of public health efforts to identify and treat TB infections, especially among high-risk populations.