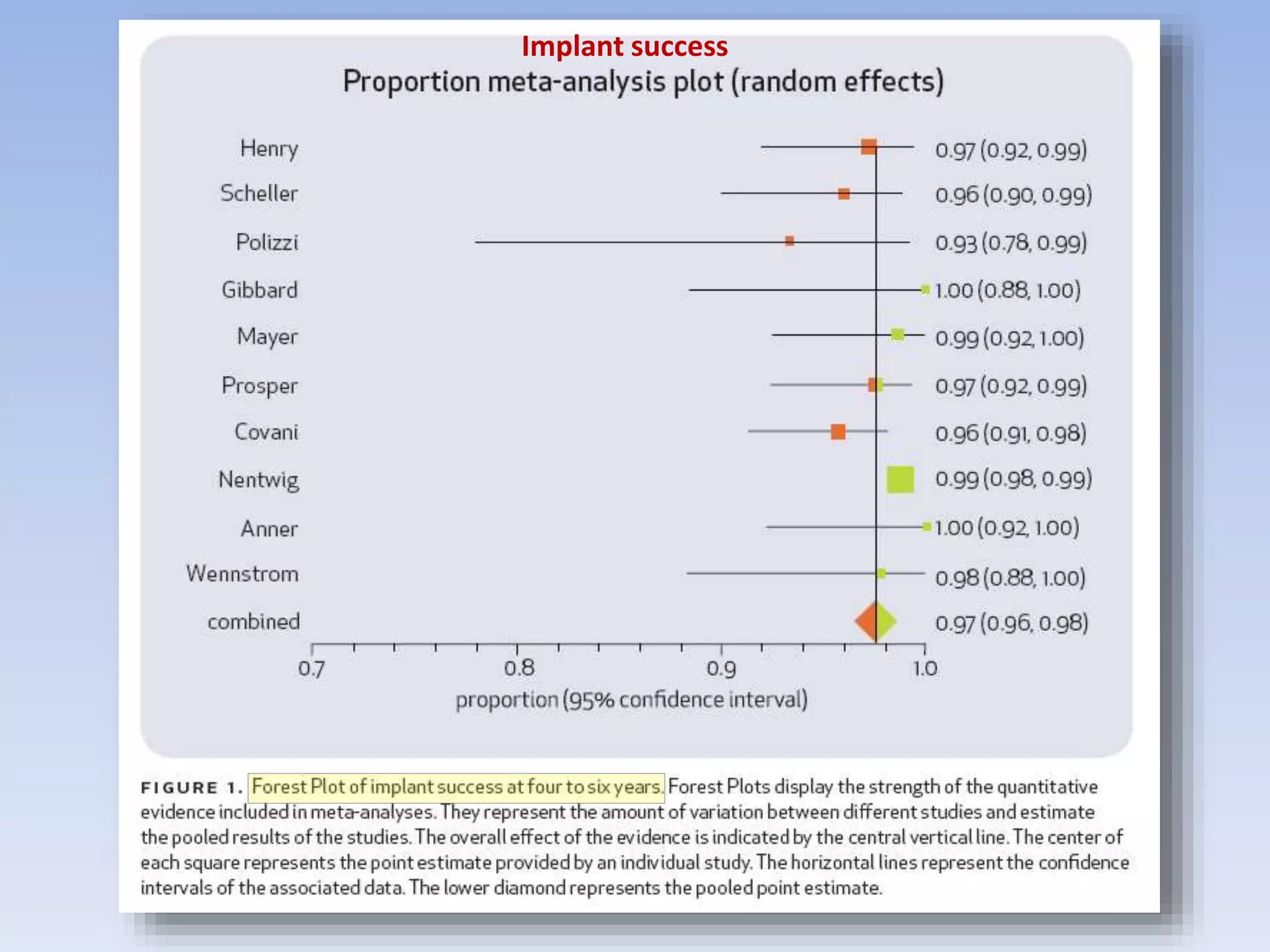
The document discusses treatment options for negative outcomes following non-surgical root canal treatment, including non-surgical retreatment, surgical retreatment, and dental implants. It reviews evidence on success rates for each option from various studies. Non-surgical retreatment can have a high success rate, particularly when there is no periapical lesion present initially. However, surgical retreatment and implants may be better options in some cases, such as when non-surgical retreatment has already failed or the anatomy makes non-surgical approaches difficult. The quality of the original root canal treatment and subsequent restoration also impact the likelihood of success. Overall, all options can have high success rates when performed by skilled operators and case selection is considered