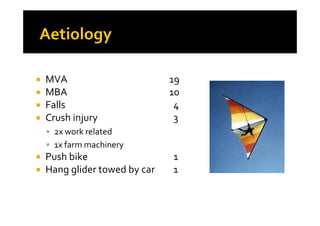
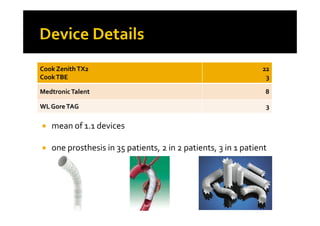
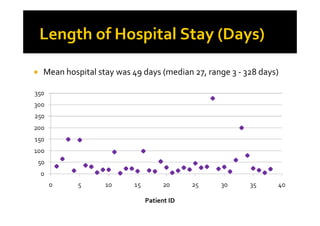
This document summarizes the establishment of a registry in Queensland, Australia to document outcomes of TEVAR (thoracic endovascular aortic repair) for traumatic aortic tears. Between 1996-2010, 38 patients underwent TEVAR for blunt traumatic aortic tears with a mean age of 43. The majority were male victims of motor vehicle or motorbike accidents. Outcomes included a low 30-day mortality rate of 2.6%, no instances of paralysis, and a low stent graft complication rate. However, follow-up was concerning with 45% lost to follow-up. The registry aims to evaluate long-term outcomes and durability of TEVAR for traumatic aortic injuries.