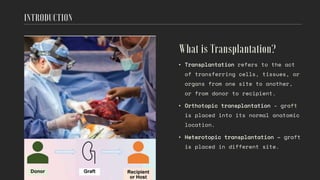
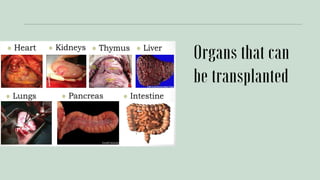
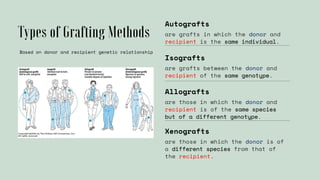
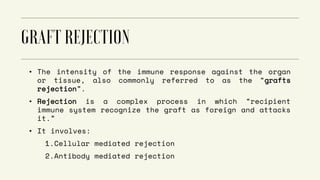
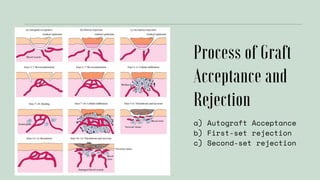
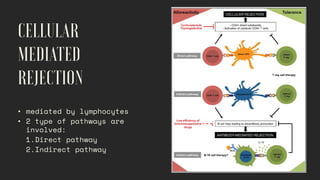
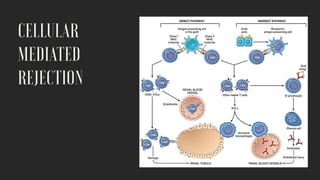
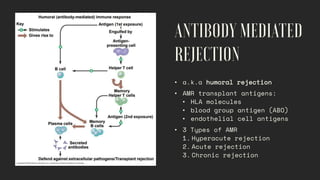
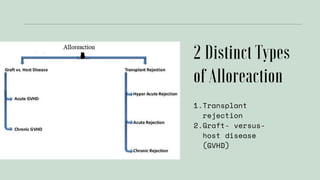
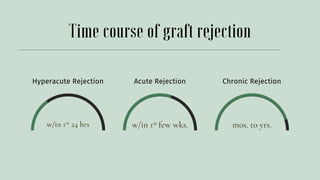
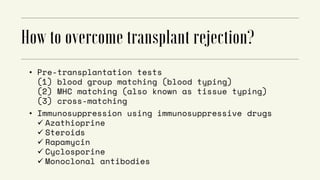
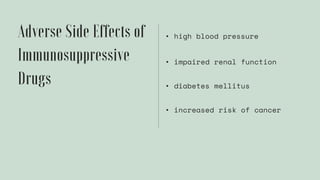
This document discusses organ transplantation and graft rejection. It describes the different types of grafts based on the genetic relationship between donor and recipient, including autografts, isografts, allografts, and xenografts. It then explains the mechanisms of graft rejection, including cellular and antibody-mediated rejection. The stages of rejection - hyperacute, acute, and chronic rejection - are also outlined. Finally, methods for overcoming transplant rejection through immunosuppression and proper donor-recipient matching are presented.