1. Transplantation immunology examines the immune response to transplanted tissues.
2. Major events include the first successful organ transplants in the 1950s-60s of kidneys, livers, hearts, and bone marrow.
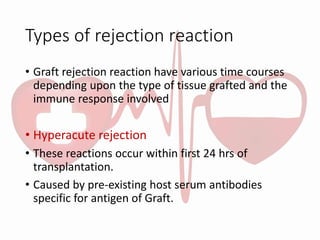
3. Graft rejection is driven by an immune response to foreign histocompatibility antigens like MHC proteins, with T-cells playing a key role through cell-mediated responses. Immunosuppressive drugs help prevent rejection by inhibiting T-cell activation and proliferation.