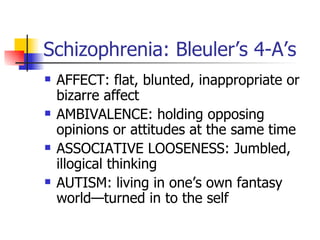
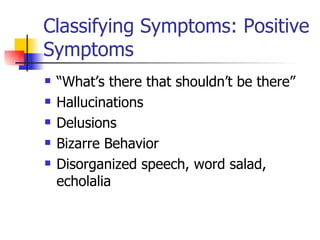
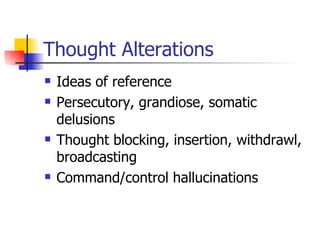
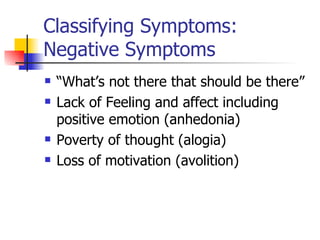
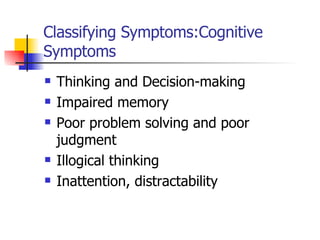
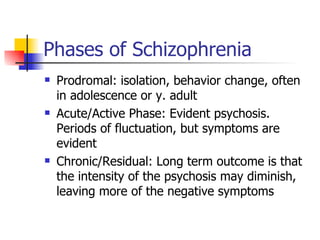
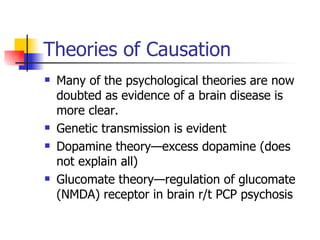
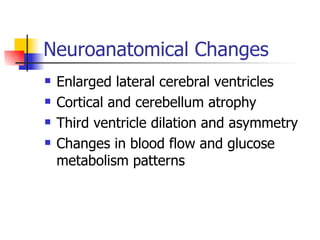
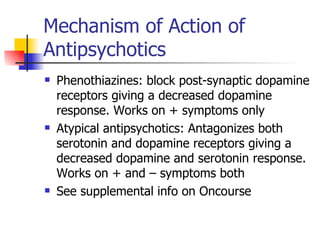
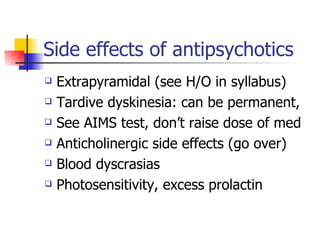
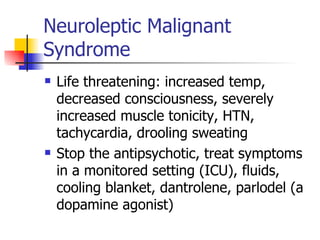
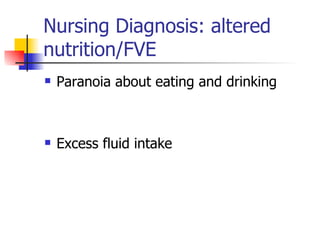
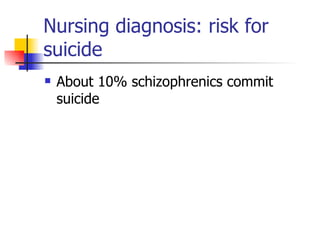
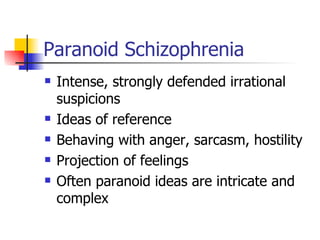
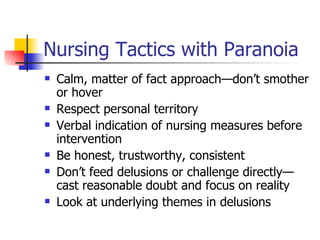
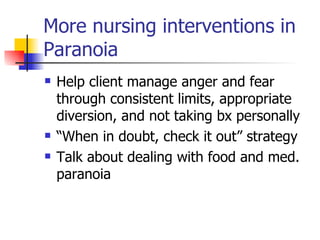
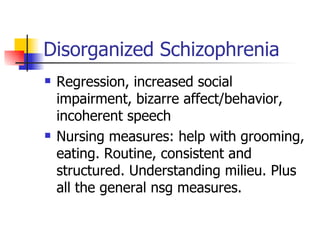
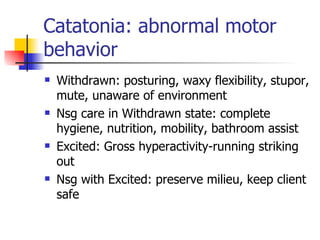
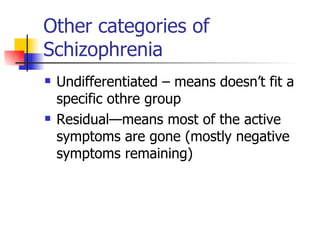
This document discusses schizophrenia and its symptoms, classifications, causes, and treatment options. It describes Bleuler's 4 A's of schizophrenia symptoms. Positive symptoms include hallucinations and delusions, while negative symptoms involve a lack of emotion and motivation. Schizophrenia progresses through prodromal, acute, and chronic phases. Antipsychotic medications work by blocking dopamine and serotonin receptors. Nursing diagnoses for schizophrenia patients include noncompliance, risk for violence, impaired social interactions, and risk for suicide. Nursing interventions aim to address symptoms, promote medication adherence, and ensure safety and self-care.