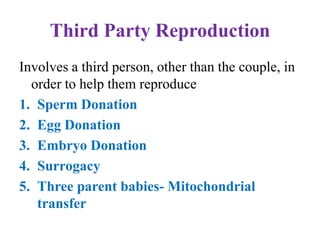
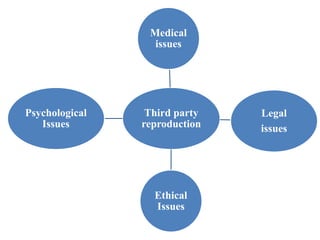
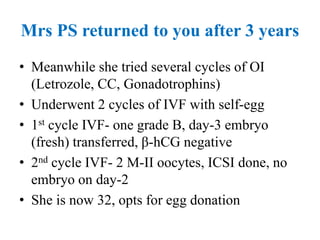
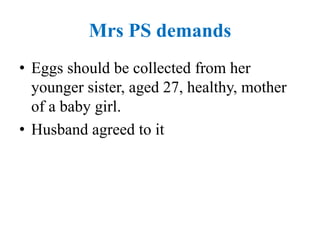
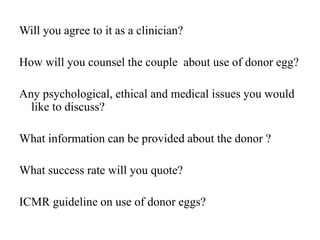
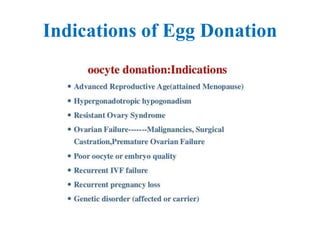
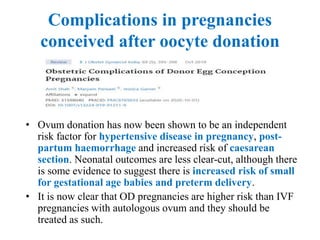
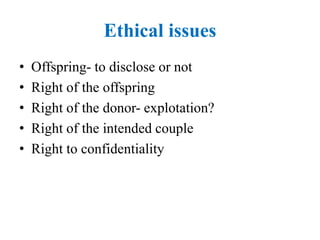
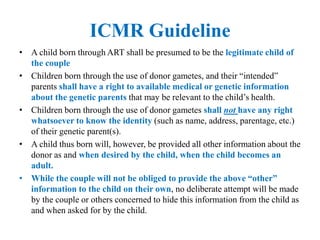
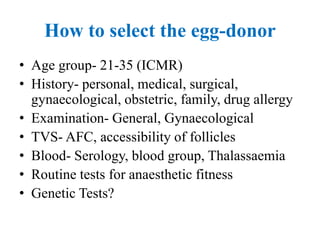
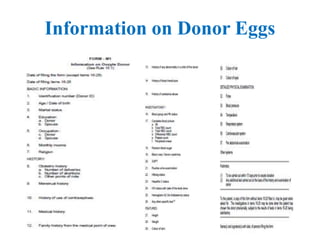
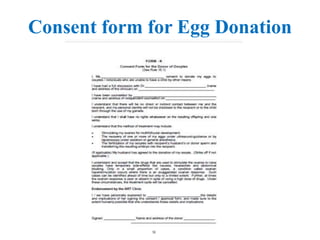
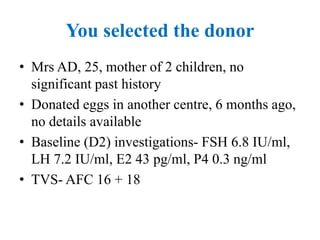
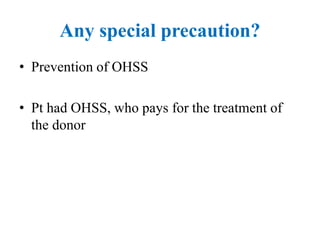
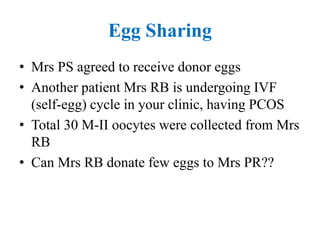
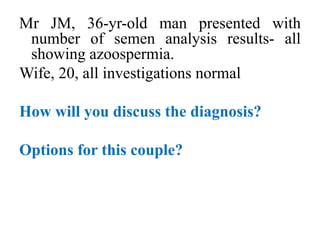
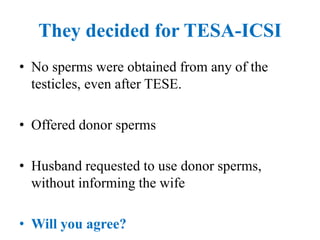
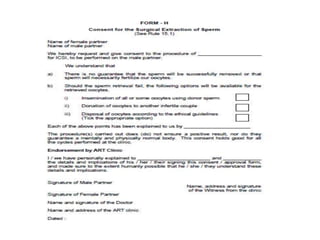
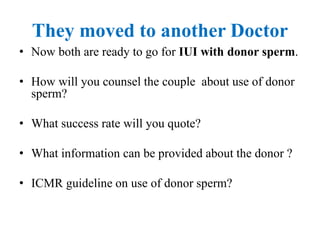
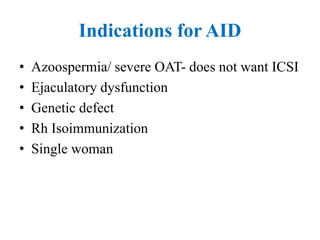
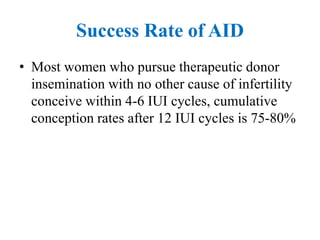
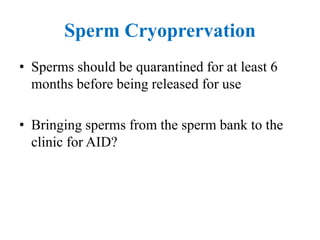
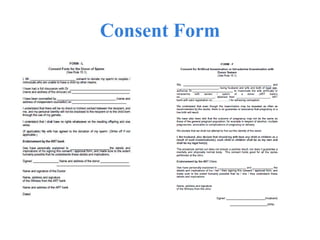
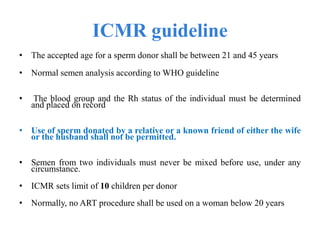
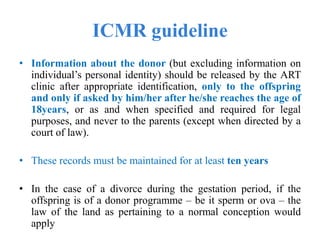
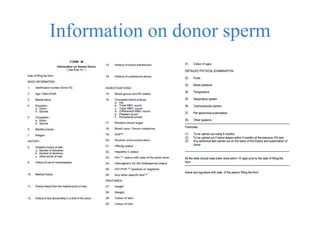
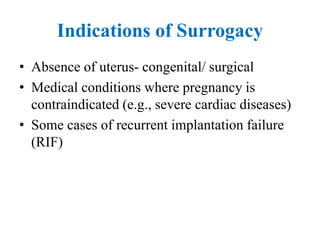
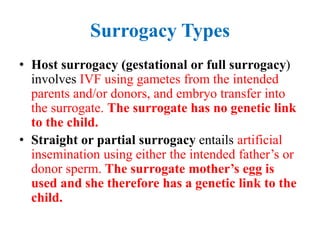
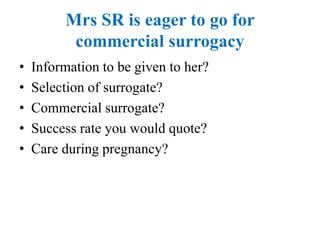
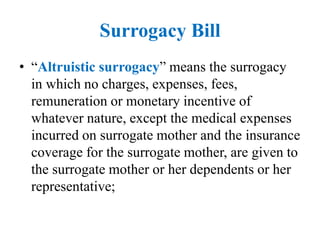
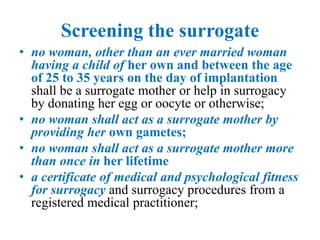
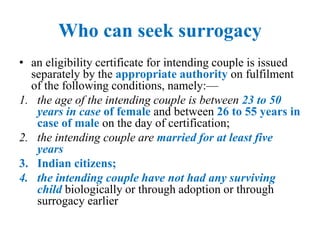
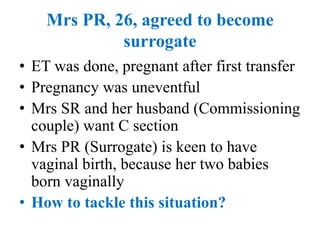
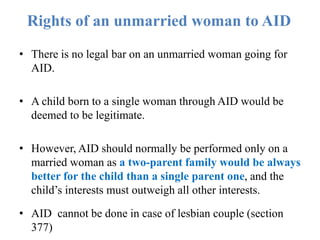
The document discusses third-party reproduction, outlining methods such as sperm, egg, and embryo donation, surrogacy, and the implications of mitochondrial transfer. It examines the medical, legal, ethical, and psychological issues associated with these practices, including case studies highlighting counseling strategies and guidelines for clinicians. Finally, it addresses the ethical considerations and guidelines from ICMR regarding donor anonymity, selection criteria, and necessary consent forms.