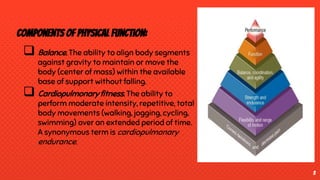
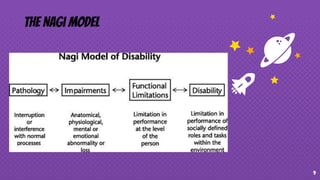
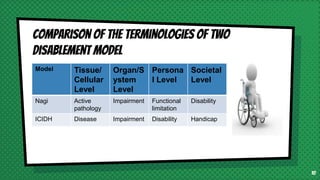
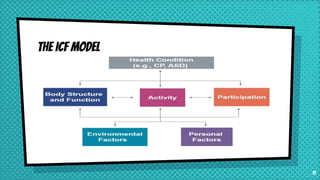
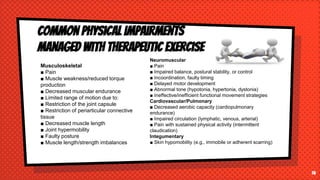
This document provides an overview of therapeutic exercise and its impact on physical function. It defines therapeutic exercise as planned bodily movements, postures, or physical activities intended to remediate or prevent impairments, improve physical function, prevent health risks, and optimize overall health. It discusses components of physical function like balance, coordination, flexibility, and muscle performance. It also covers models of disablement including the Nagi model, ICIDH model, and ICF model. Finally, it discusses common physical impairments, risk factors for disability, and types of prevention through rehabilitation.