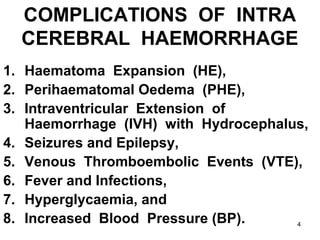
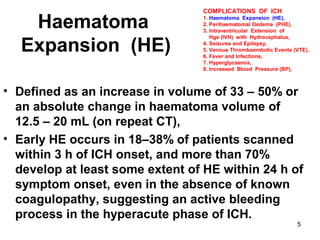
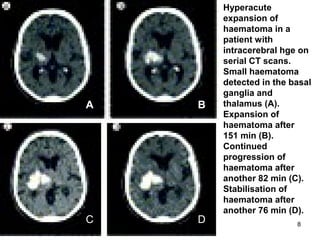
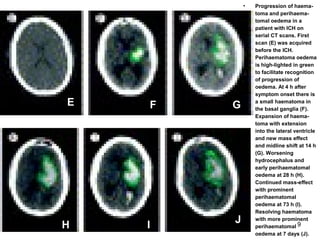
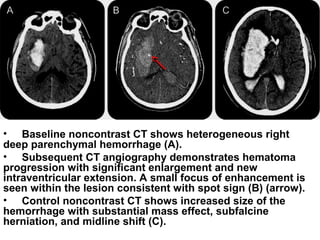
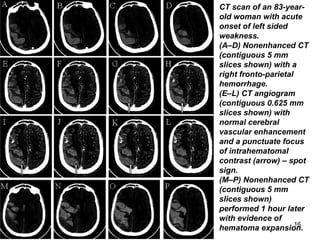
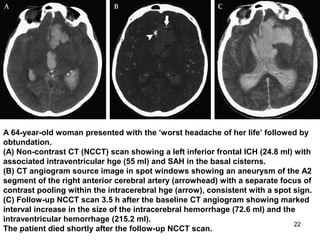
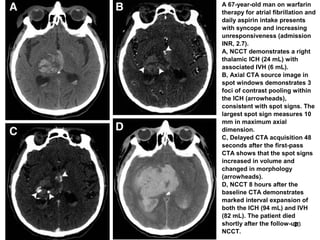
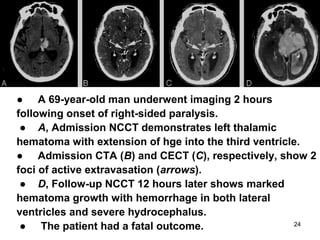
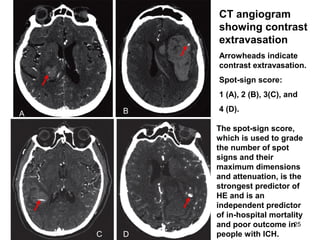
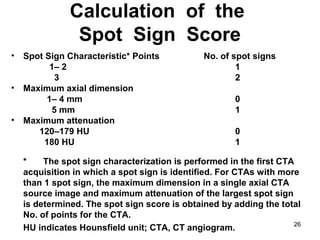
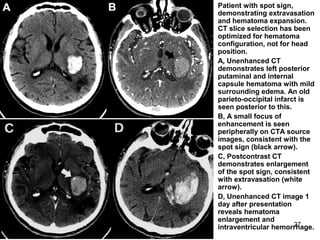
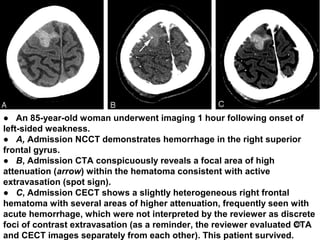
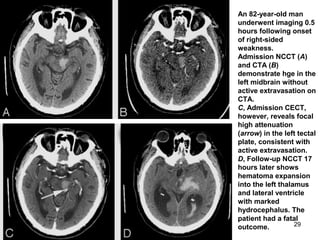
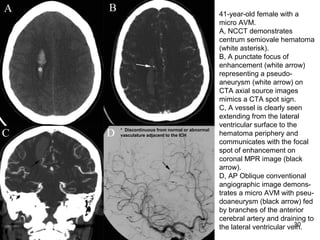
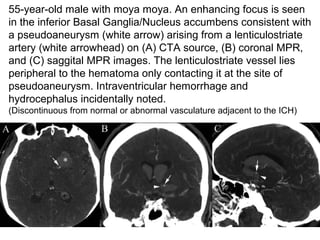
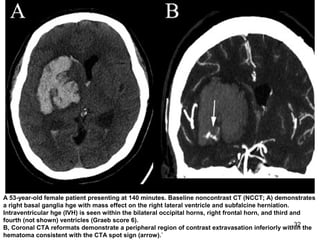
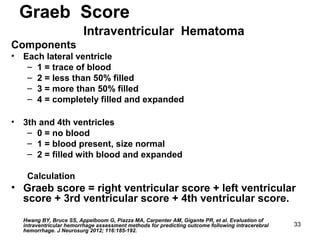
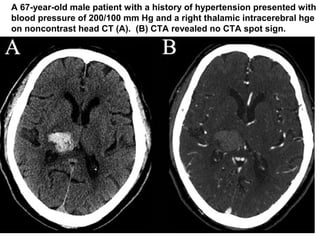
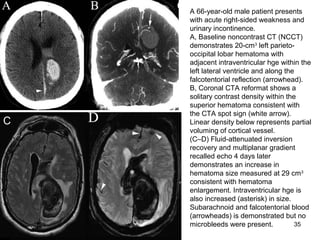
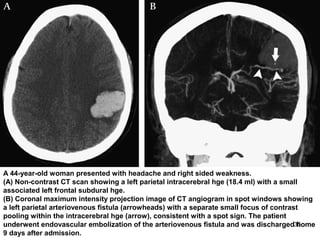
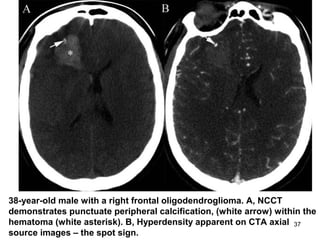
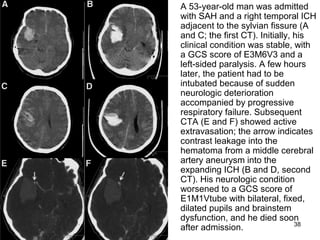
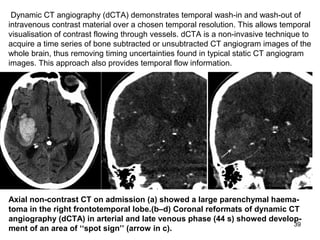
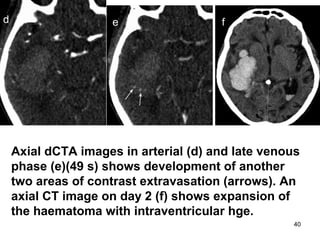
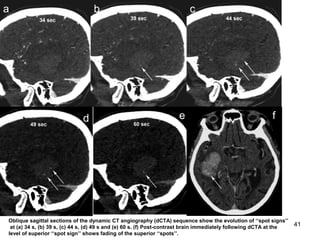
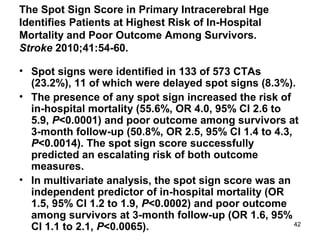
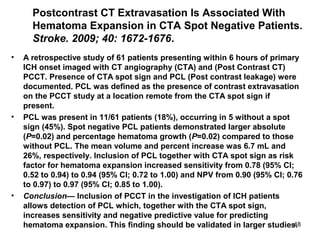
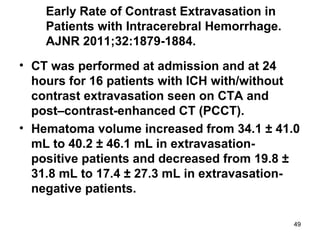
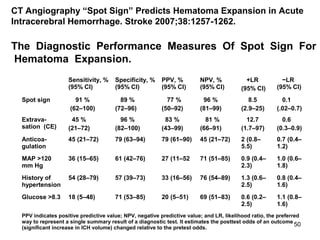
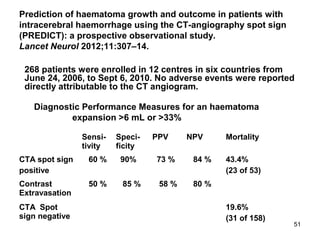
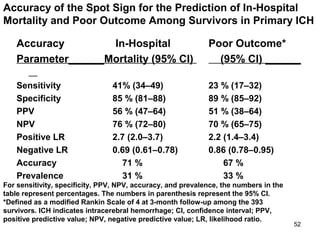
The document discusses spontaneous or primary intracerebral hemorrhage (ICH), which accounts for 10-30% of first-ever strokes, with a 30-day mortality rate of 30-55%. It highlights complications such as hematoma expansion, which increases the risk of poor outcomes and mortality, and the importance of the 'spot sign' in identifying patients at higher risk of significant hematoma expansion and death. Multi-detector CT angiography (MDCTA) is emphasized as a preferred diagnostic tool due to its speed, accuracy, and lower risk compared to conventional methods.