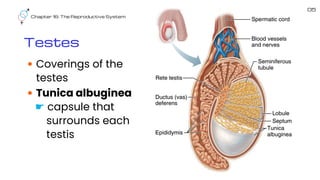
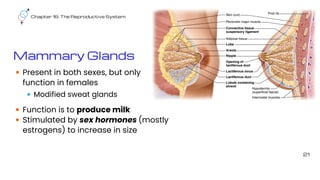
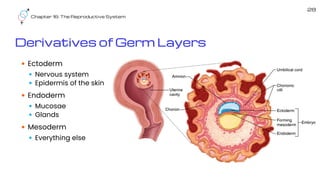
The document provides a comprehensive overview of the male and female reproductive systems, detailing the structures and functions of various reproductive organs, including gonads, testes, ovaries, and accessory glands. It explains the processes of spermatogenesis, oocyte fertilization, and embryonic development, along with the physiological changes during pregnancy and childbirth. Key hormonal influences, such as testosterone and estrogen, and the stages of labor are also outlined.