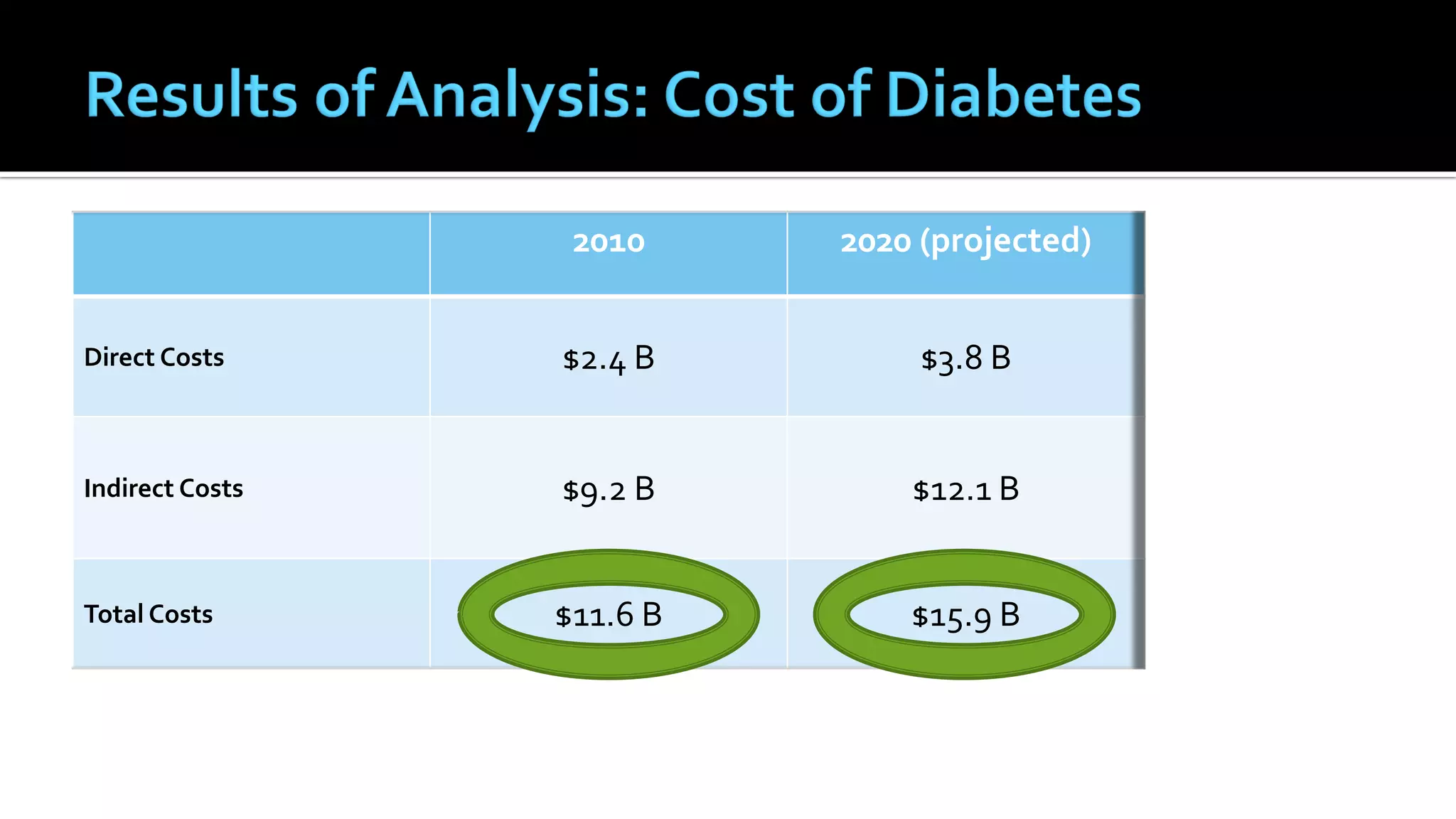
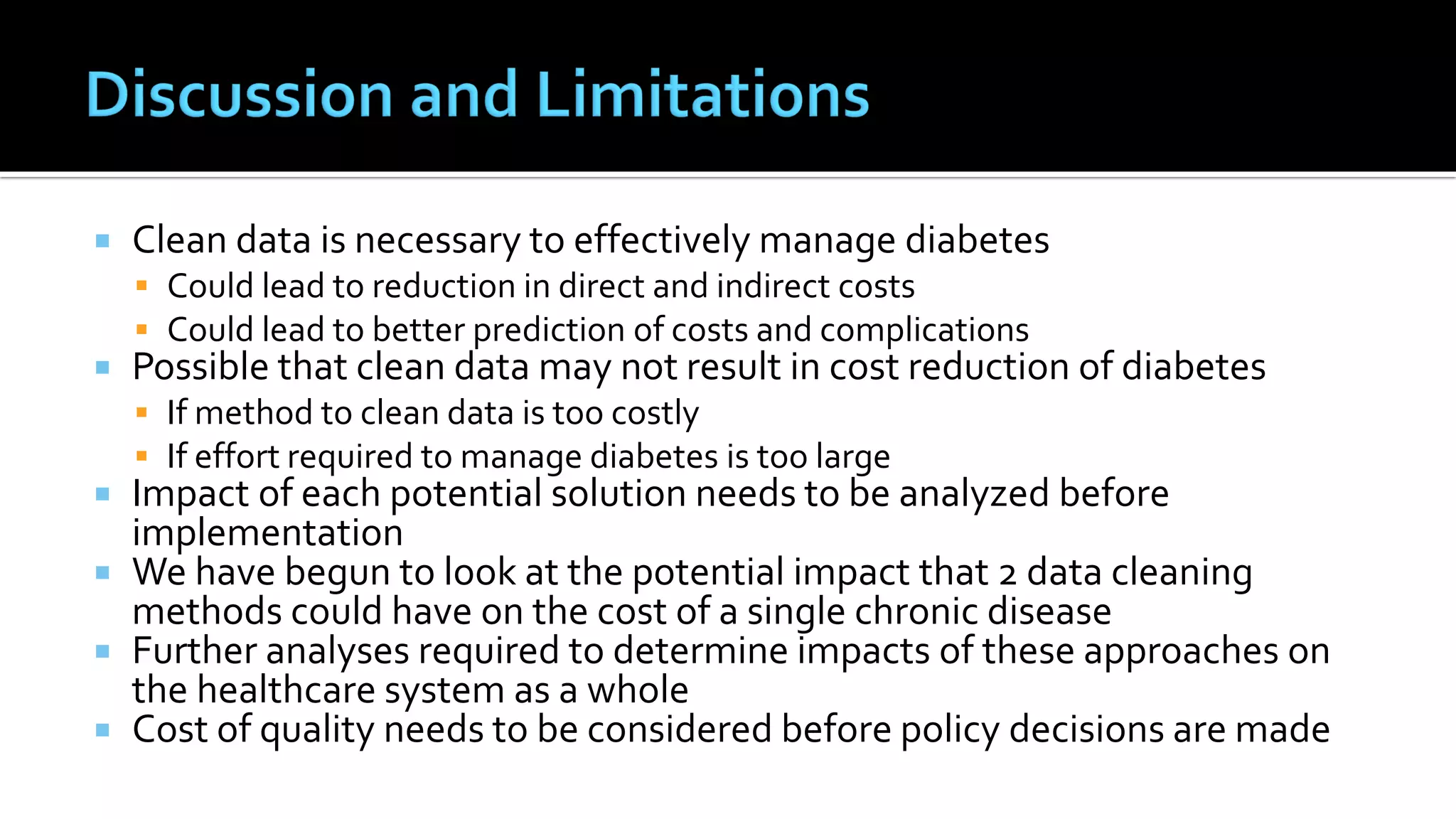
1) The document analyzes the costs of two approaches to obtaining clean data from electronic medical records (EMRs) - data discipline and data cleansing - and applies this to diabetes management in Canada.
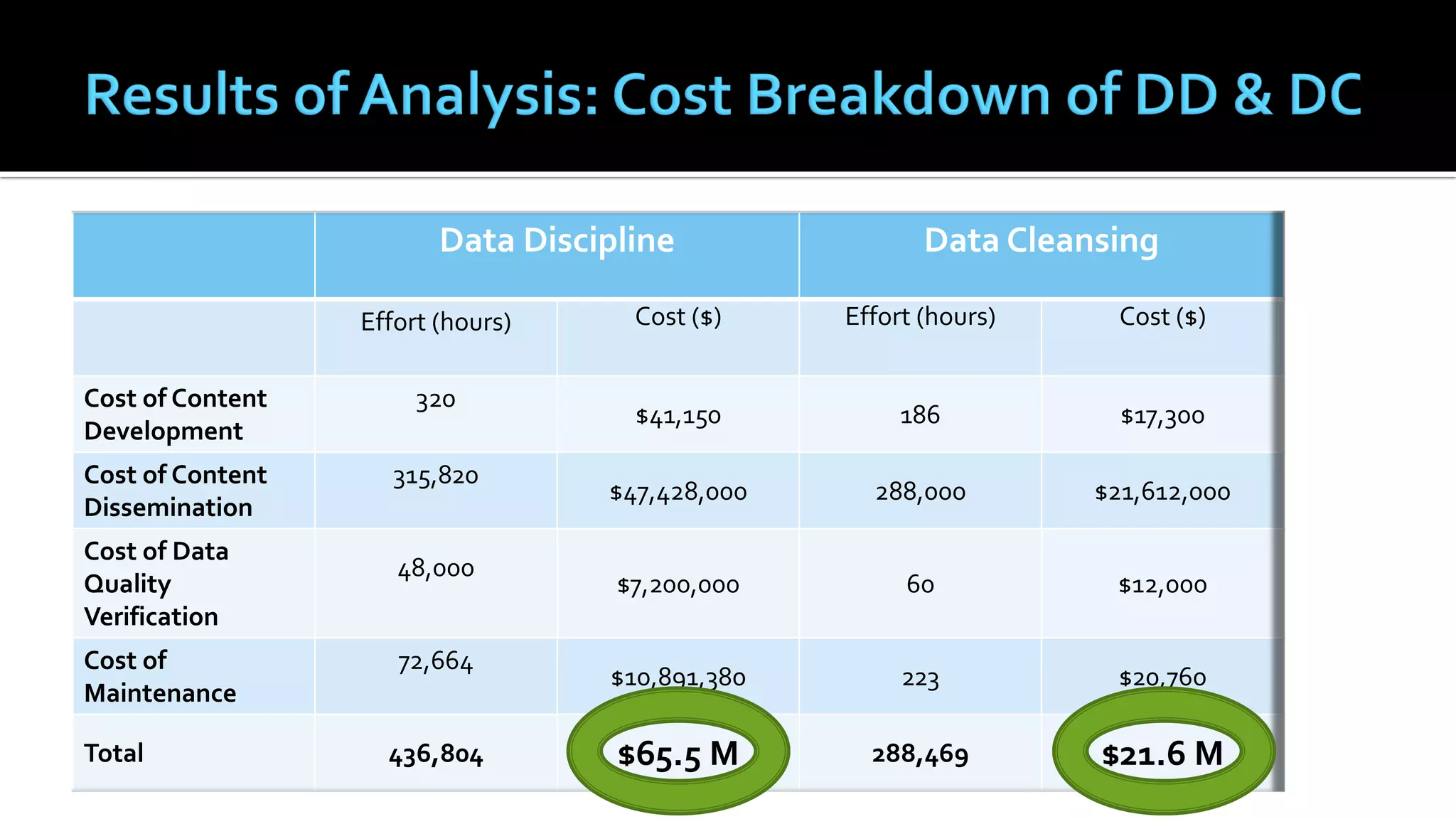
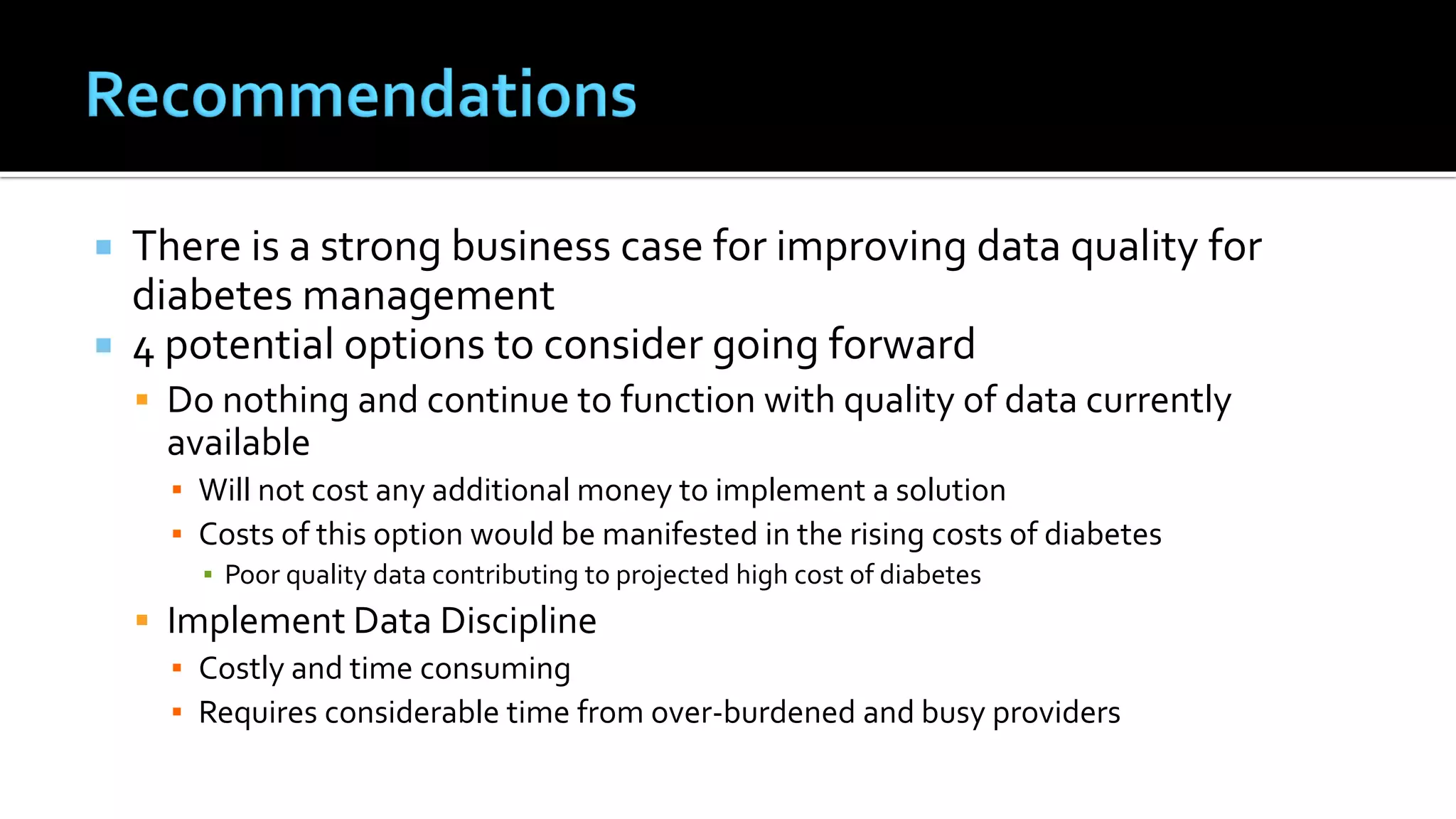
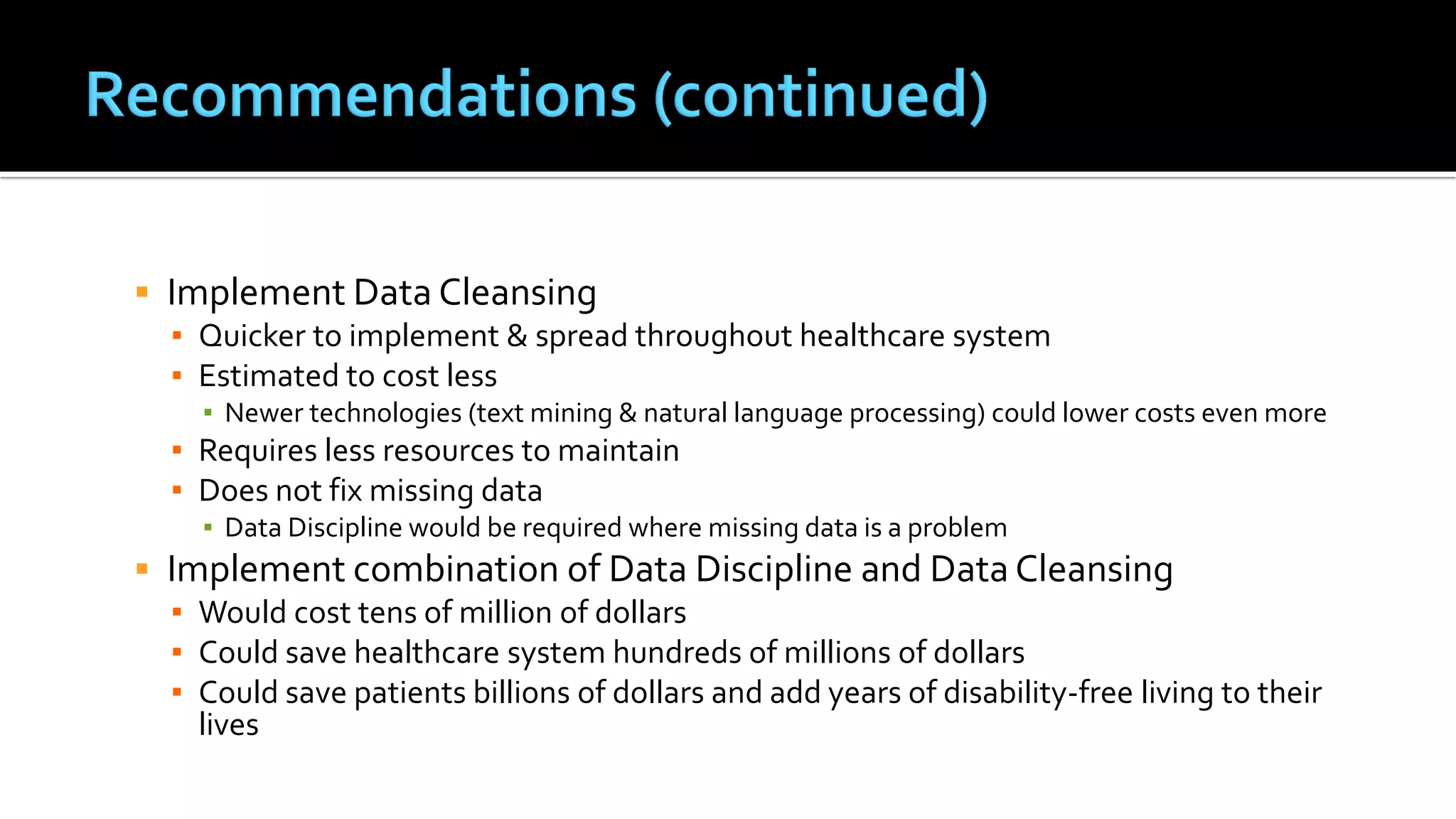
2) A budget impact analysis finds that data cleansing would be quicker to implement and estimated to cost less at $21.6 million compared to $65.5 million for data discipline.
3) The analysis recommends considering a combination of the two approaches to improve data quality for diabetes management, which could save hundreds of millions to the healthcare system and billions to patients through reduced costs and improved health.