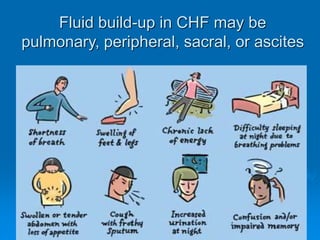
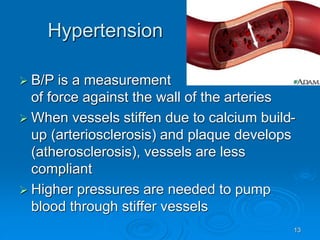
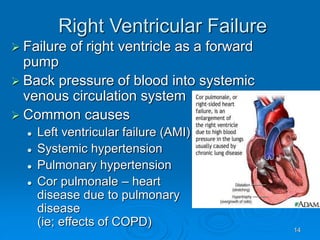
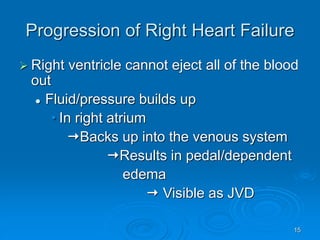
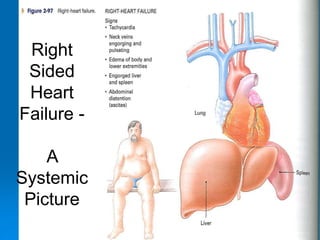
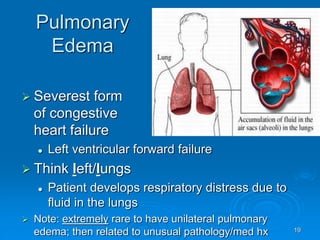
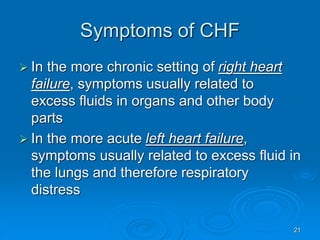
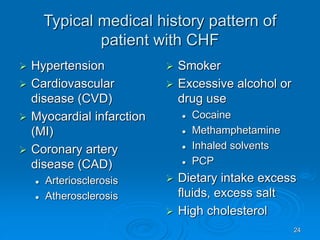
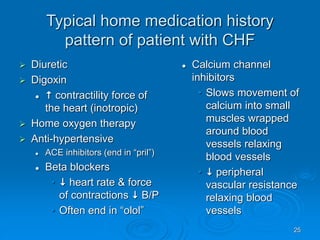
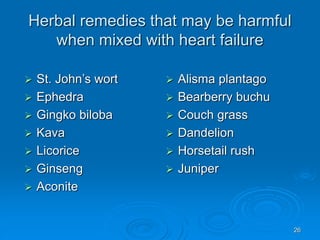
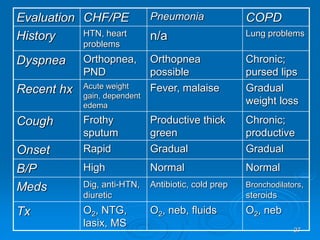
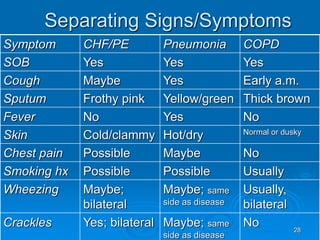
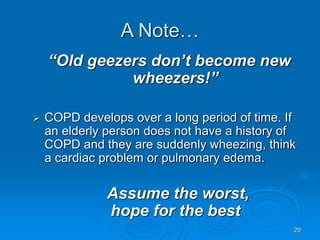
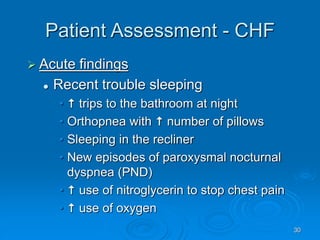
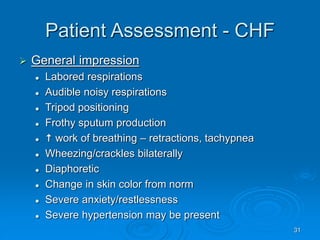
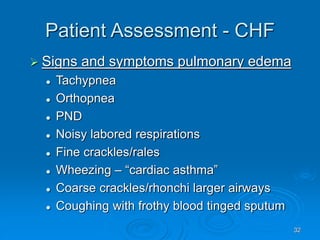
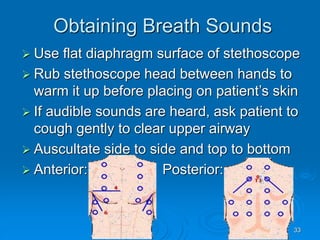
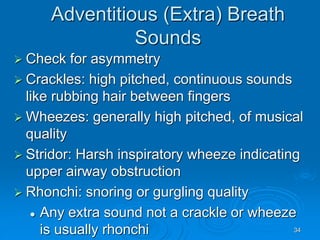
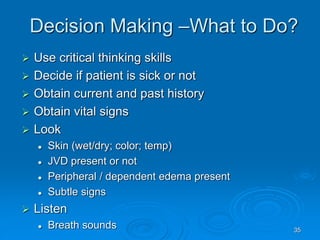
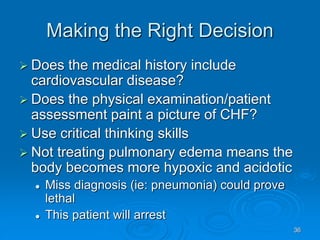
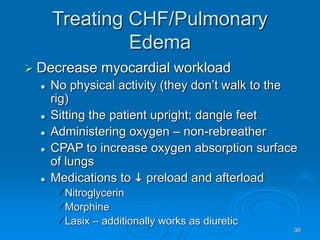
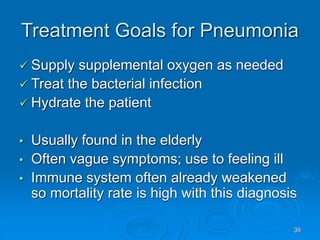
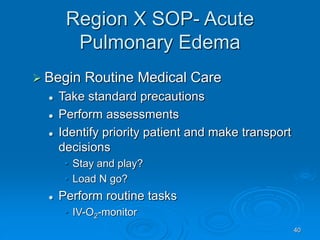
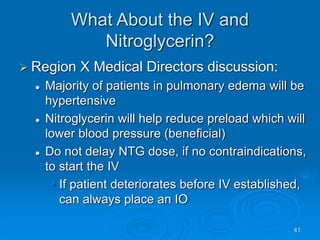
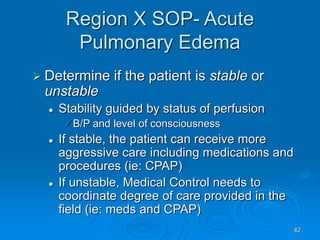
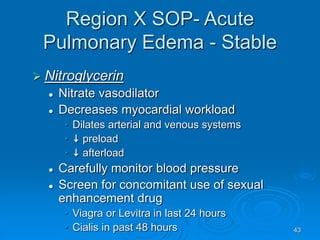
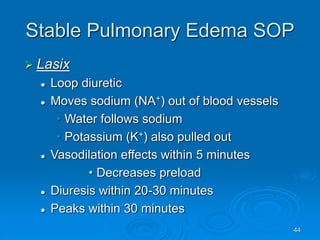
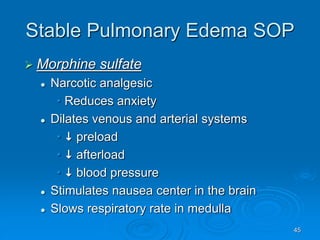
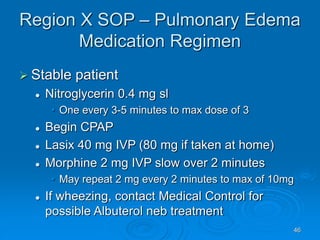
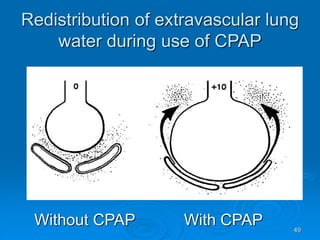
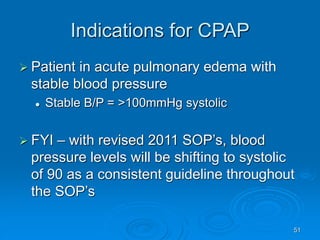
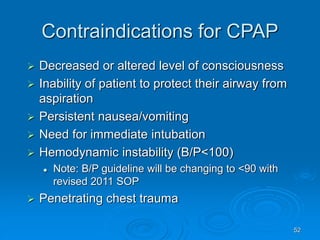
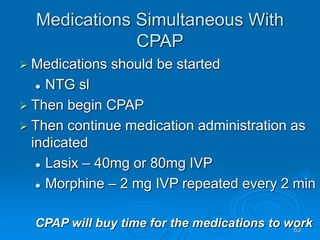
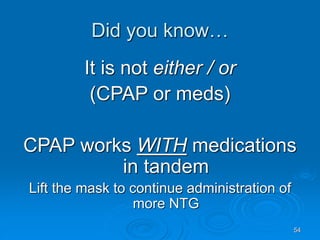
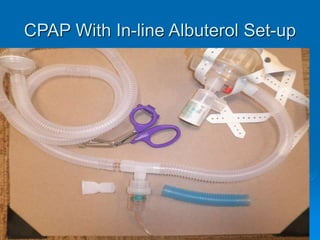
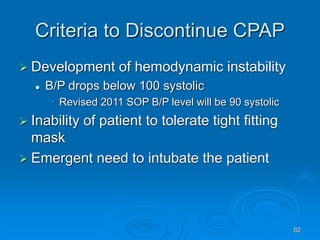
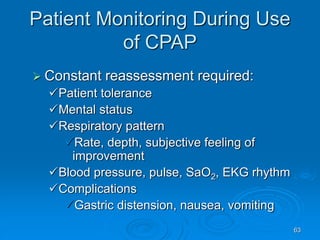
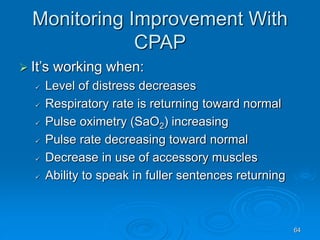
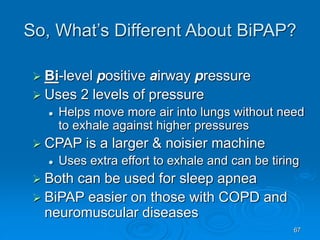
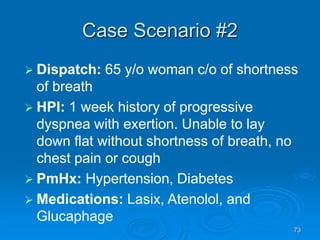
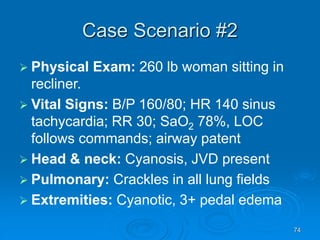
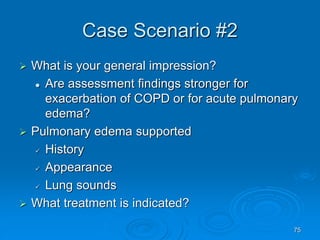
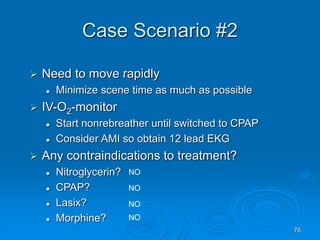
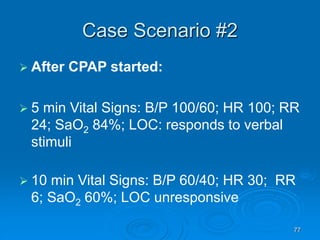
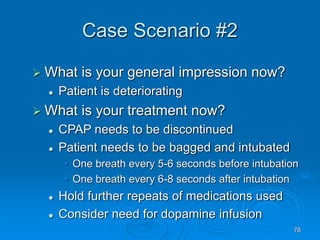
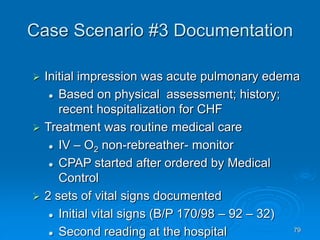
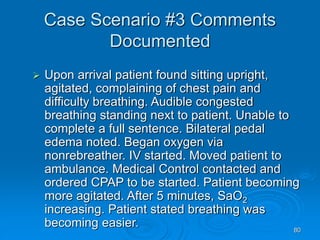
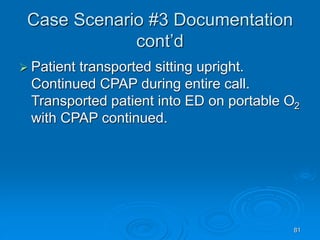
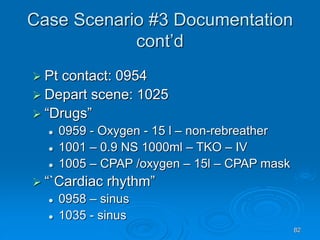
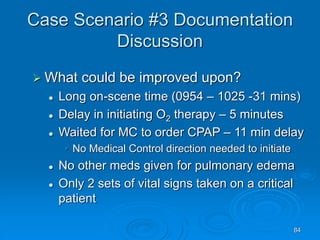
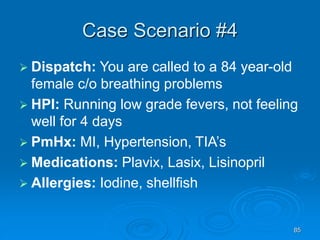
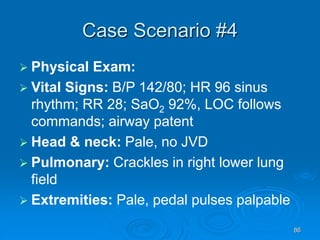
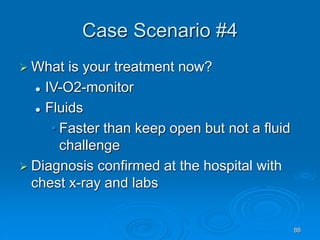
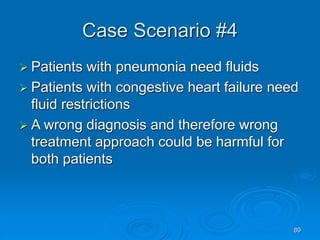
This document outlines the objectives and procedures for EMS providers regarding heart failure and the use of CPAP as an intervention. It details definitions, causes, symptoms, assessment techniques, and treatment protocols for patients with congestive heart failure and pulmonary edema. Additionally, it covers medication management, CPAP set-up, benefits, and clinical decision-making processes.