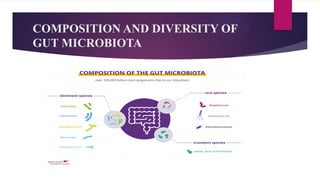
The document discusses the gut-brain axis, highlighting the bidirectional communication and influence between gut microbiota and mental health. It emphasizes the role of gut microbiota in neurotransmitter regulation, the impact of dysbiosis on various mental health disorders, and potential therapeutic interventions such as probiotics and dietary modifications. Furthermore, it explores associations between gut microbiota composition and conditions like depression, Alzheimer's disease, and neurodevelopmental disorders.