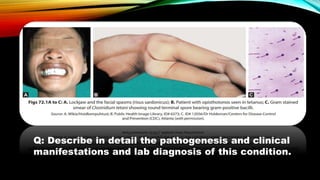
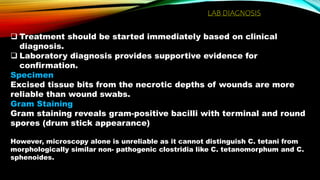
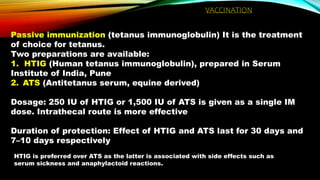
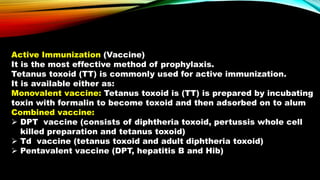
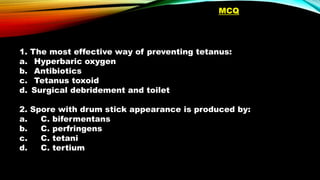
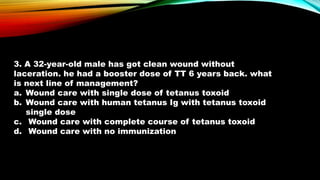
A person developed trismus, muscle pain and stiffness, back pain, and difficulty swallowing 3-5 days after a bullet injury. Examination of excised tissue from the wound revealed gram-positive bacilli with terminal and spherical spores. This is consistent with Clostridium tetani, which causes tetanus. Tetanus toxin blocks GABA inhibition in the central nervous system, causing painful muscle spasms. The most effective prevention is vaccination with tetanus toxoid.