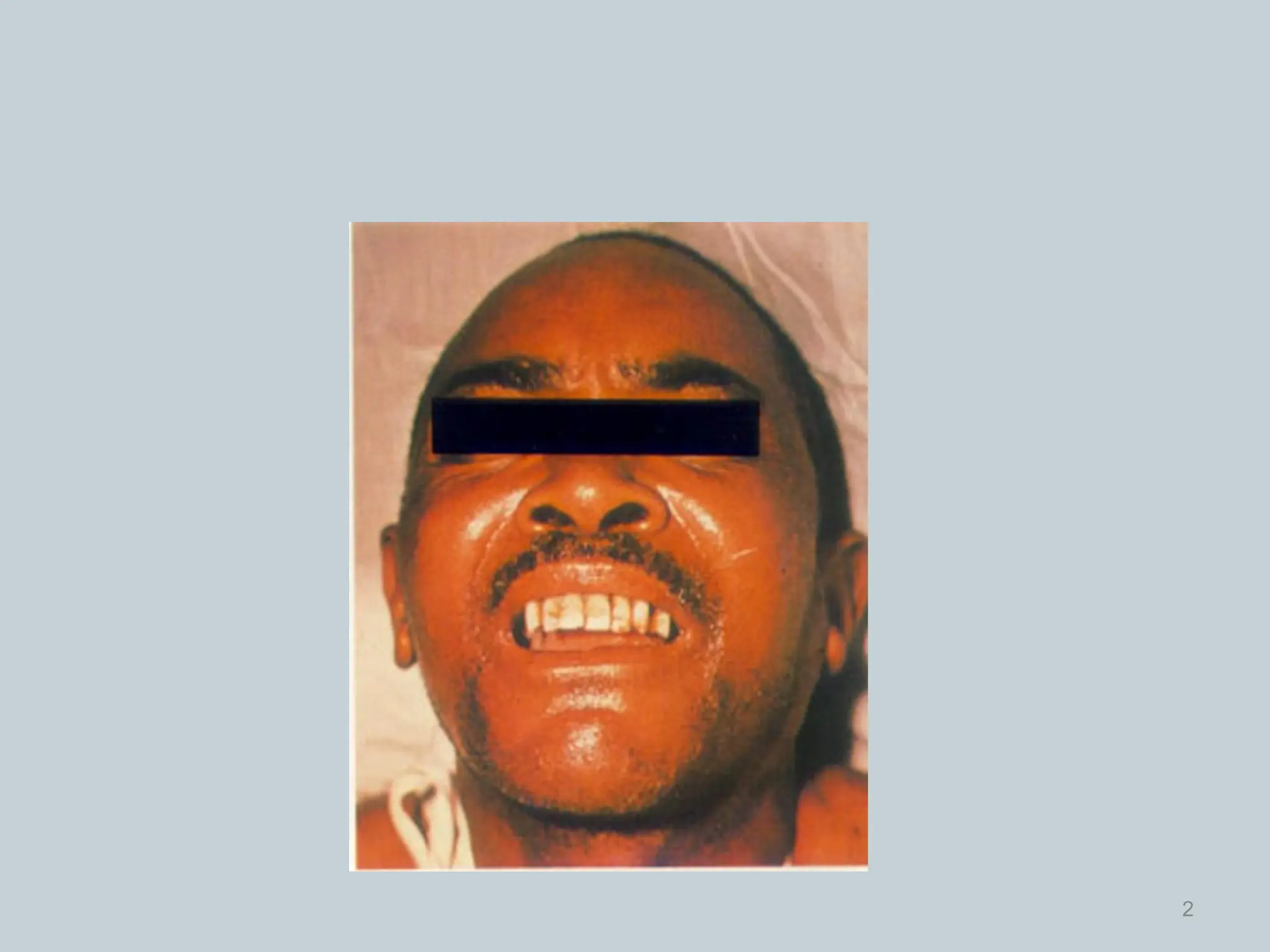
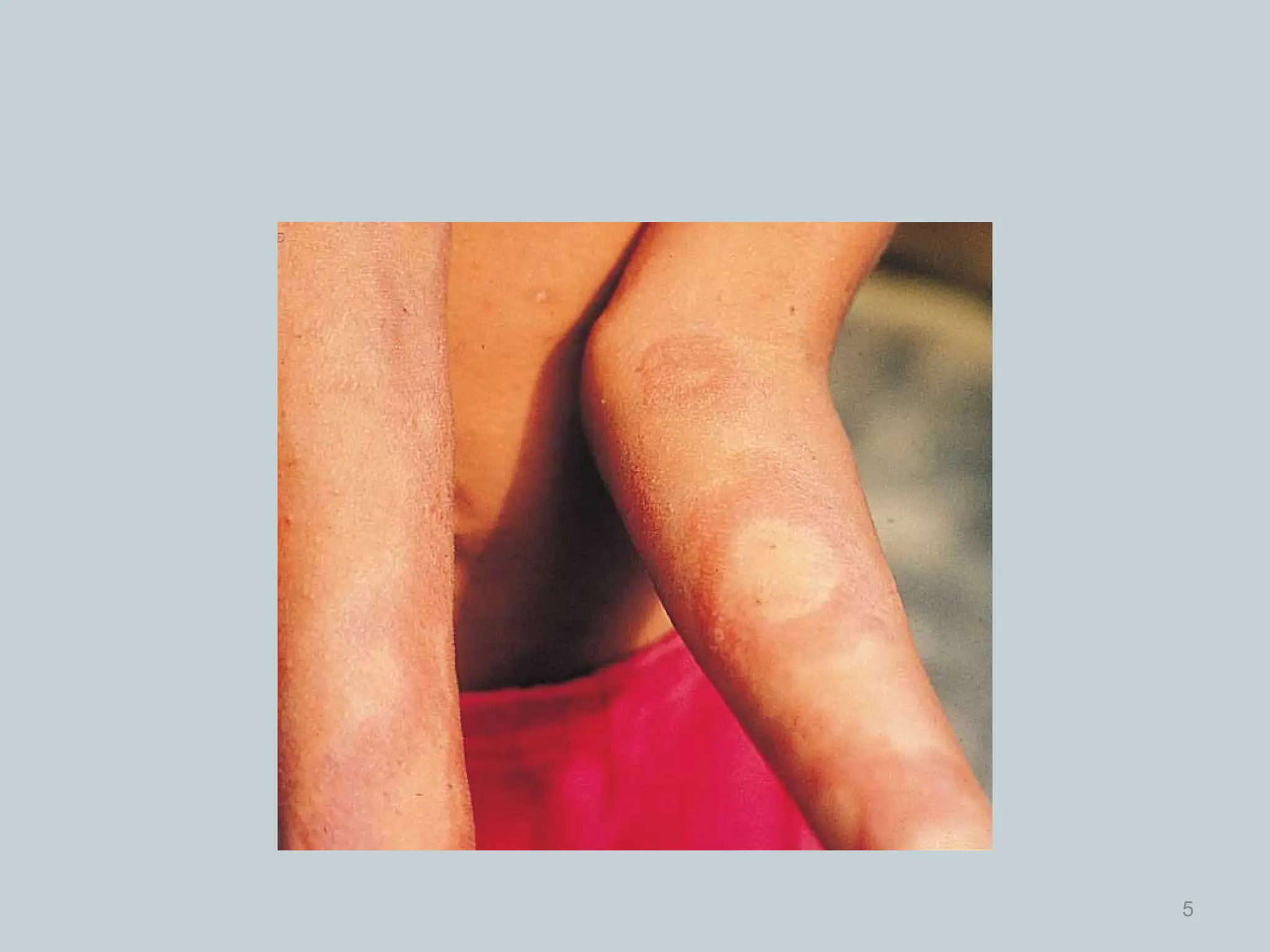
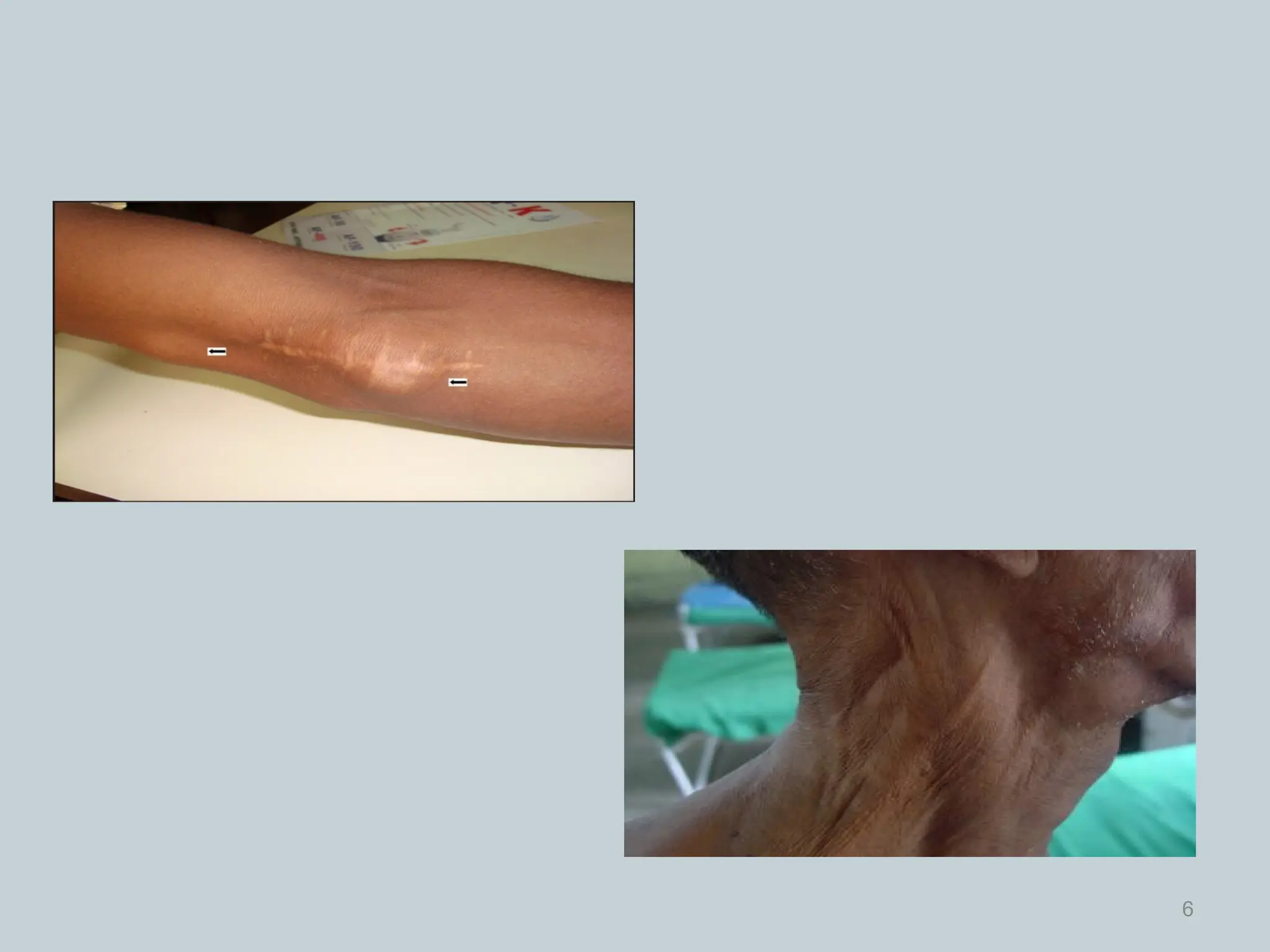
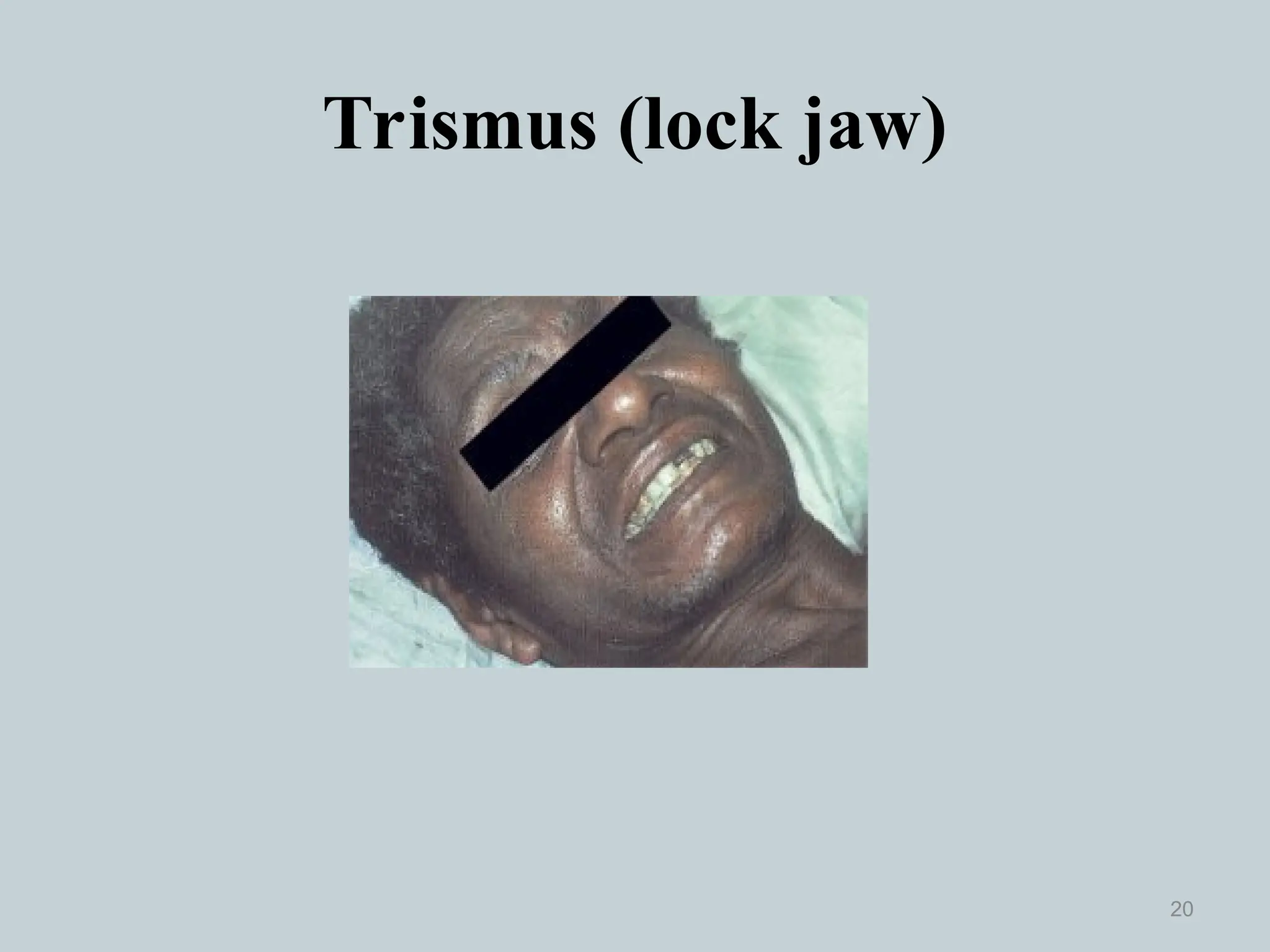
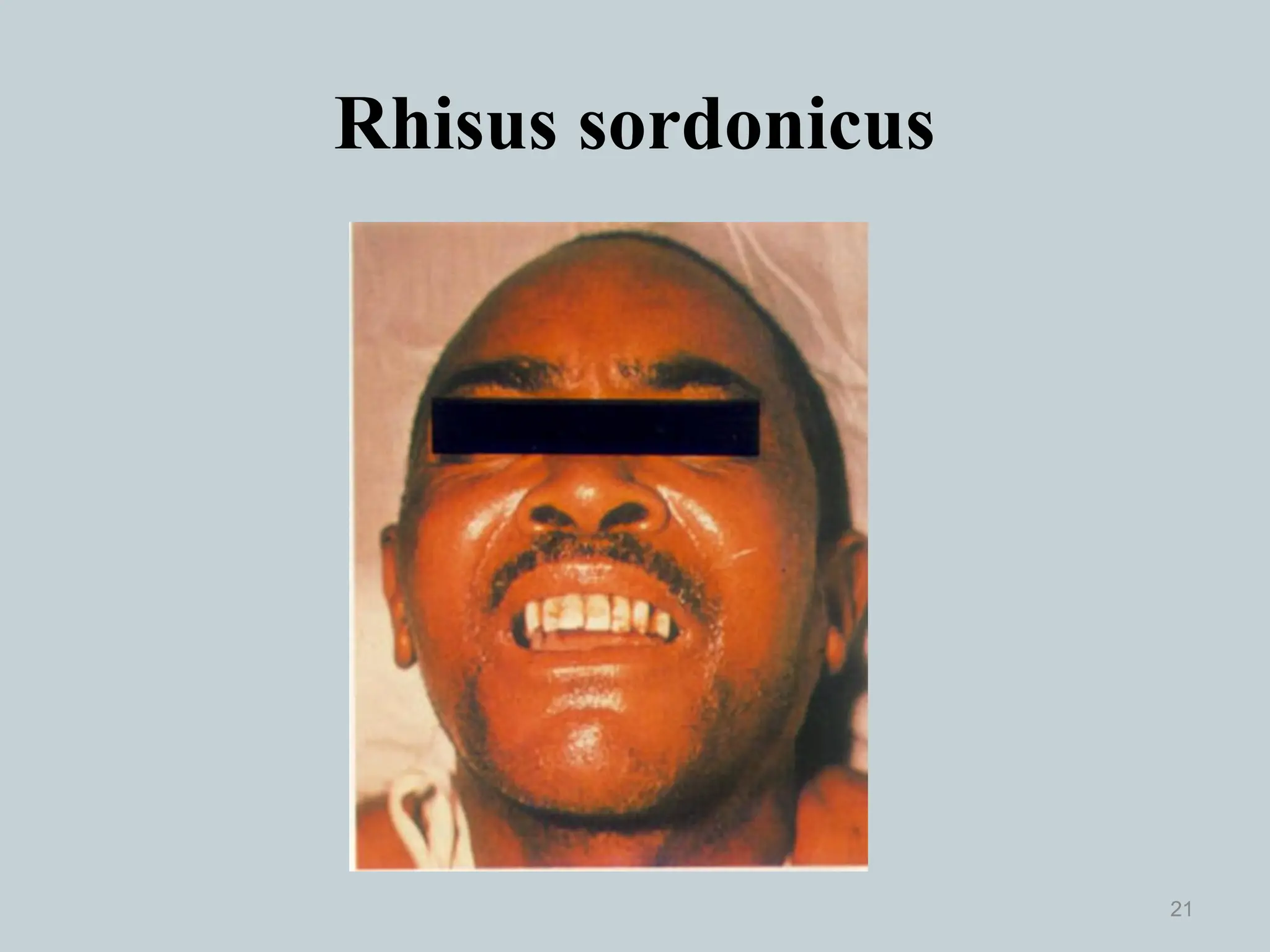
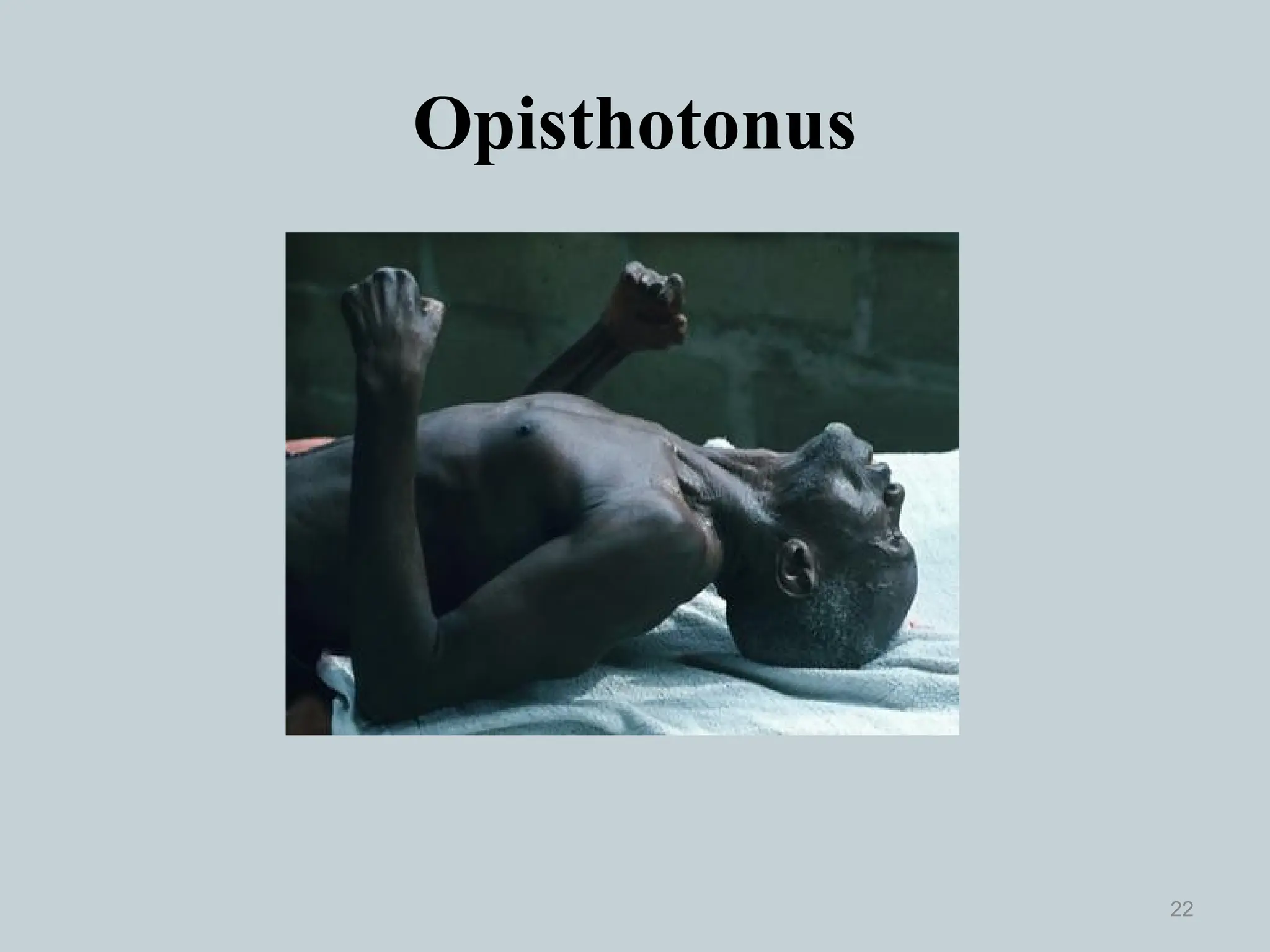
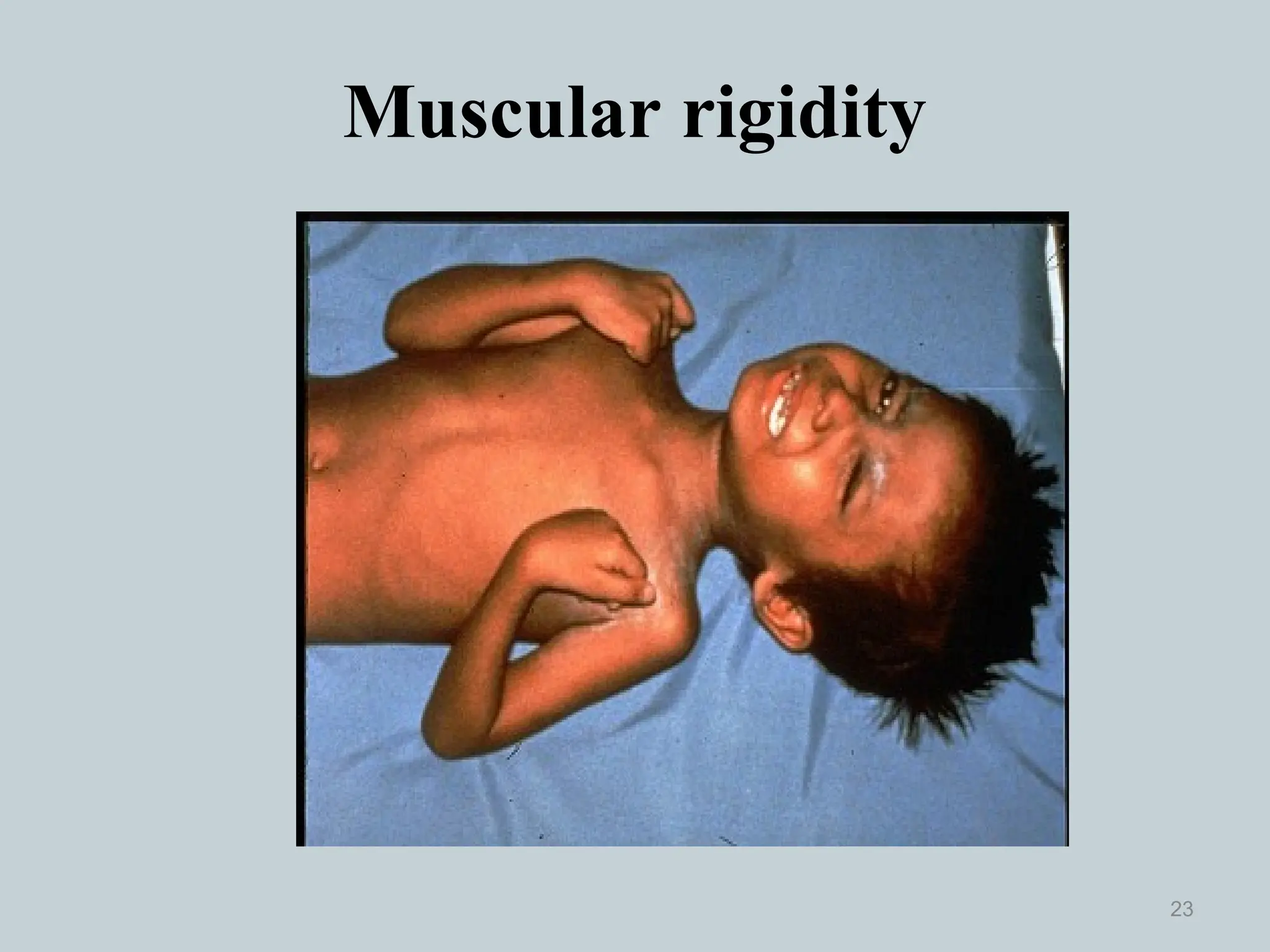
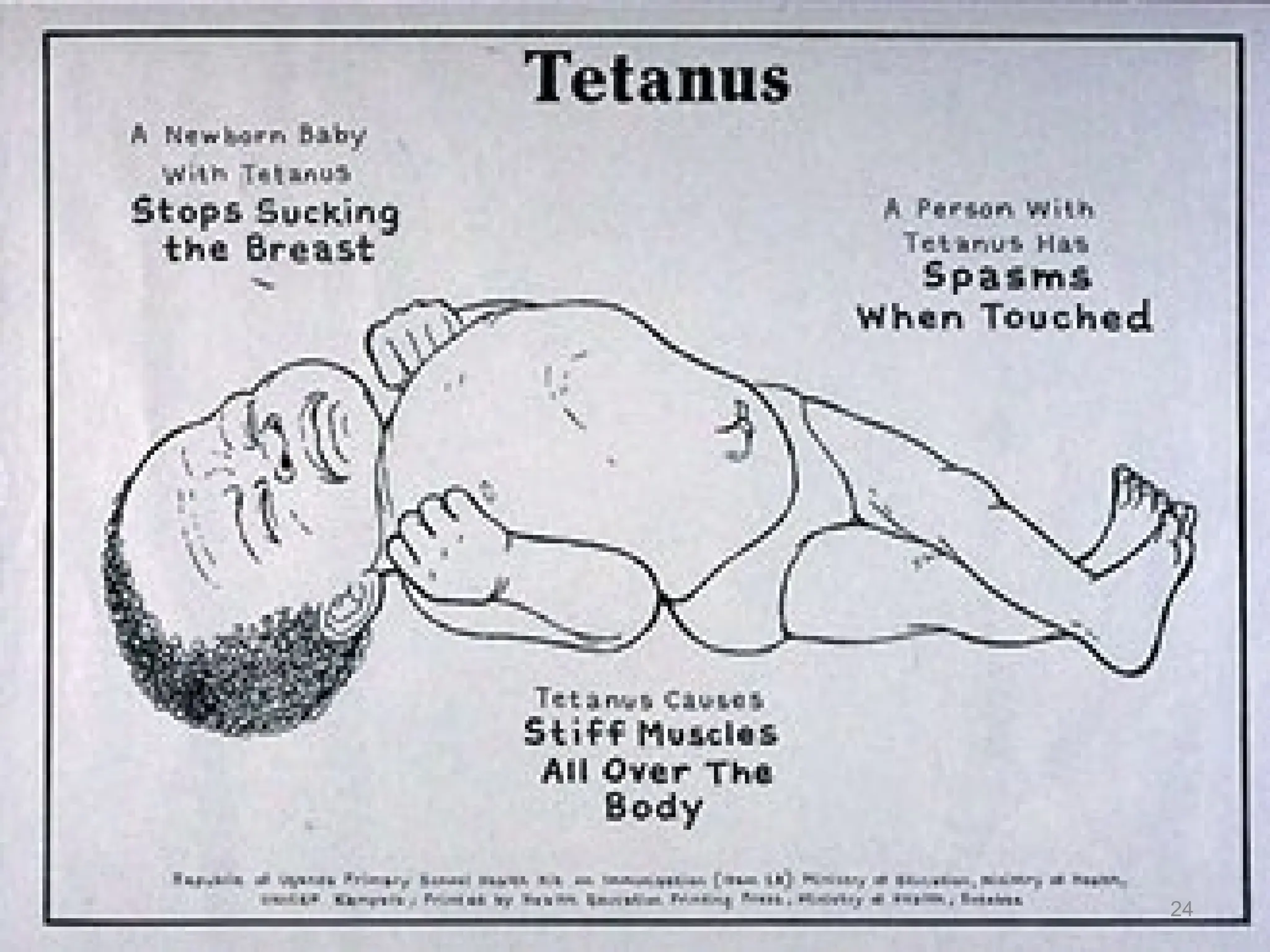
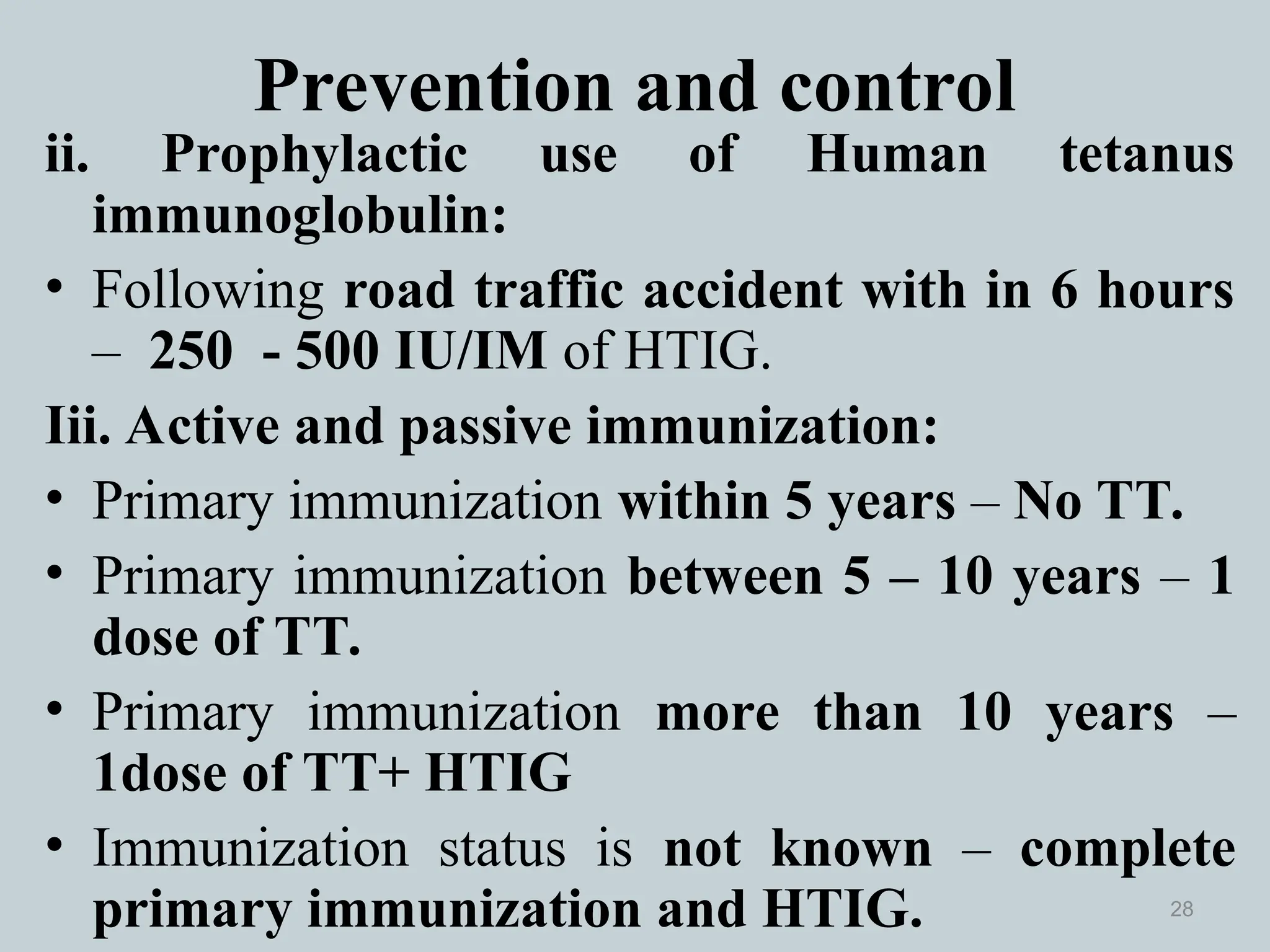
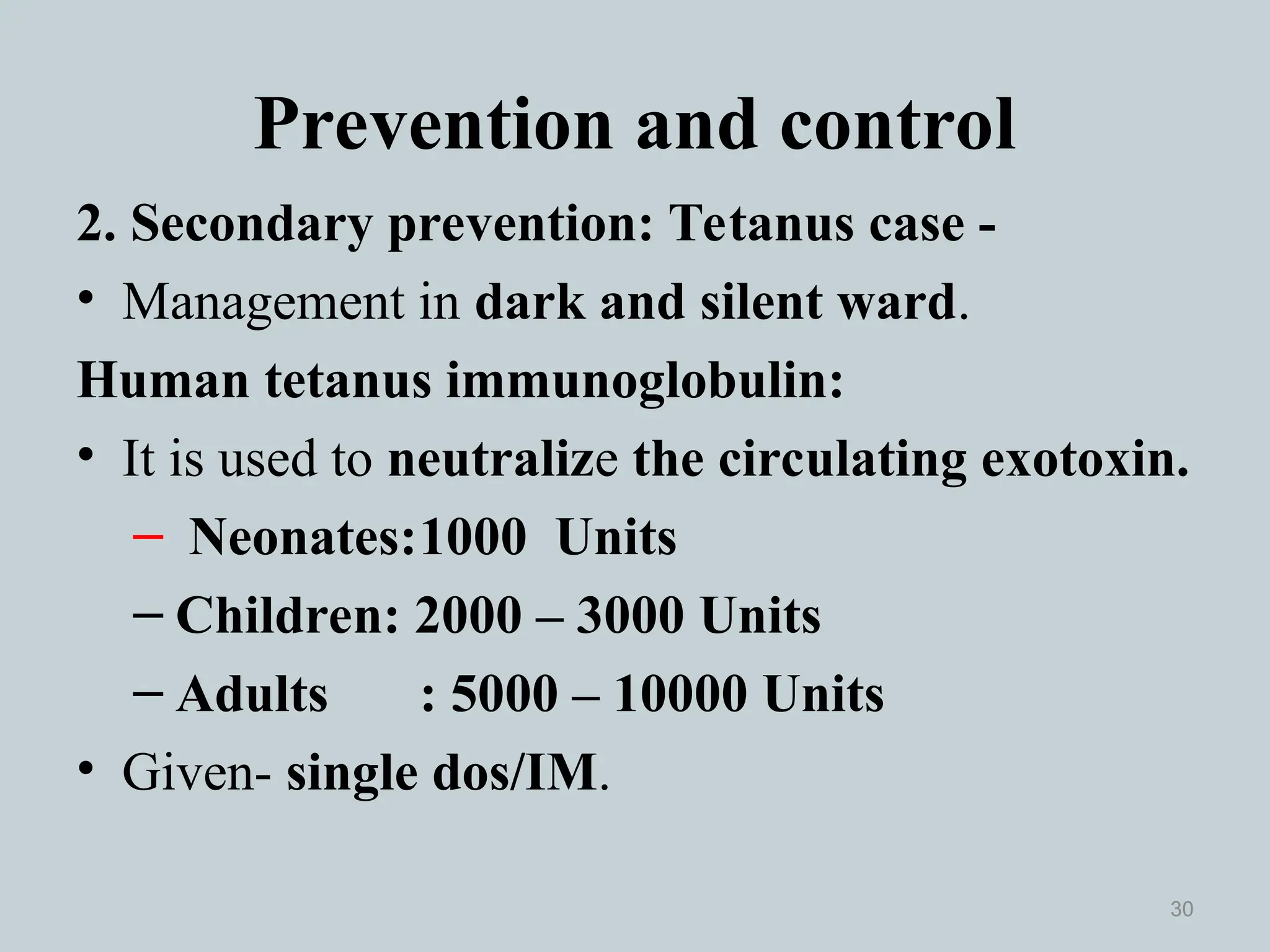
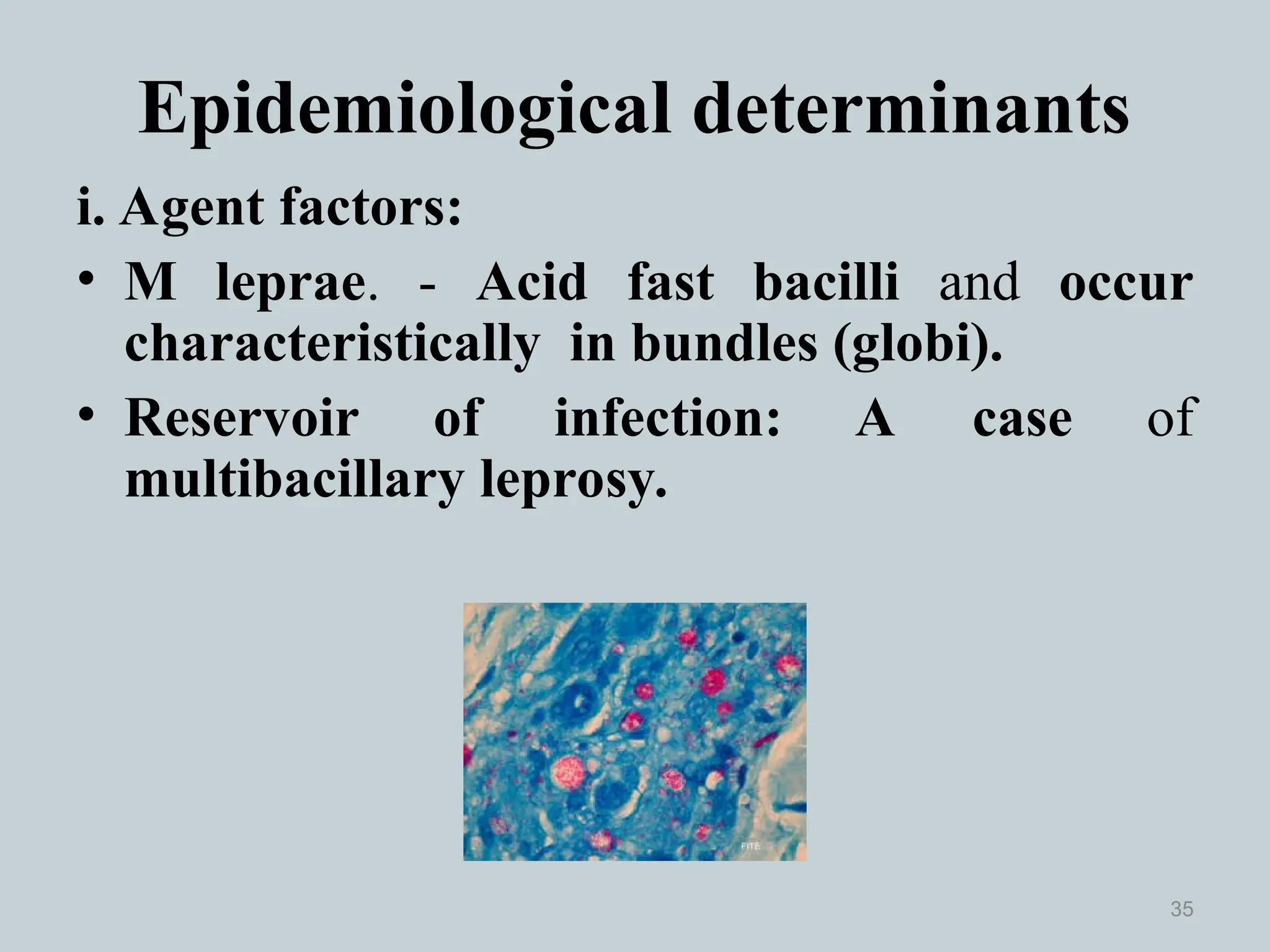
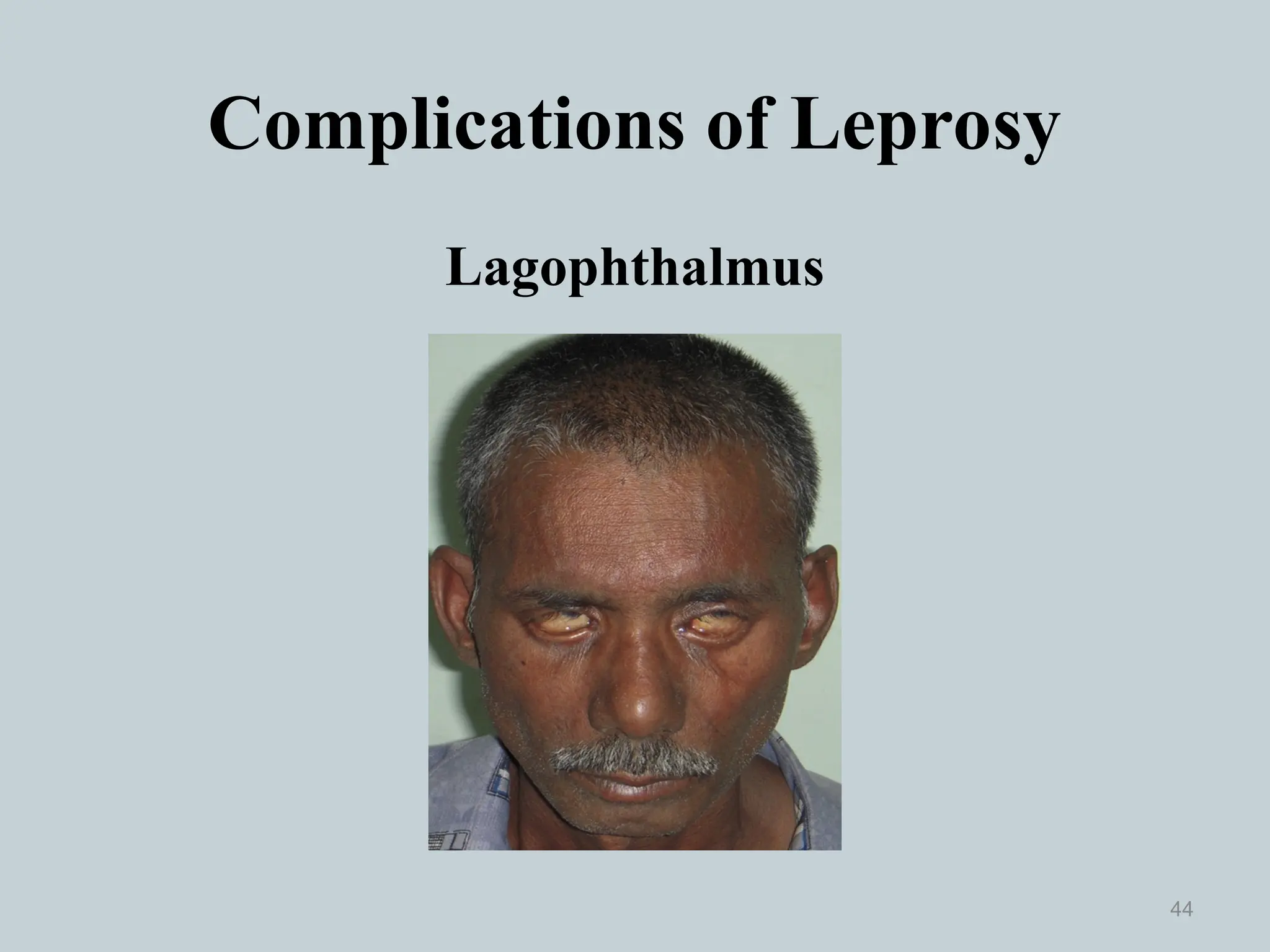
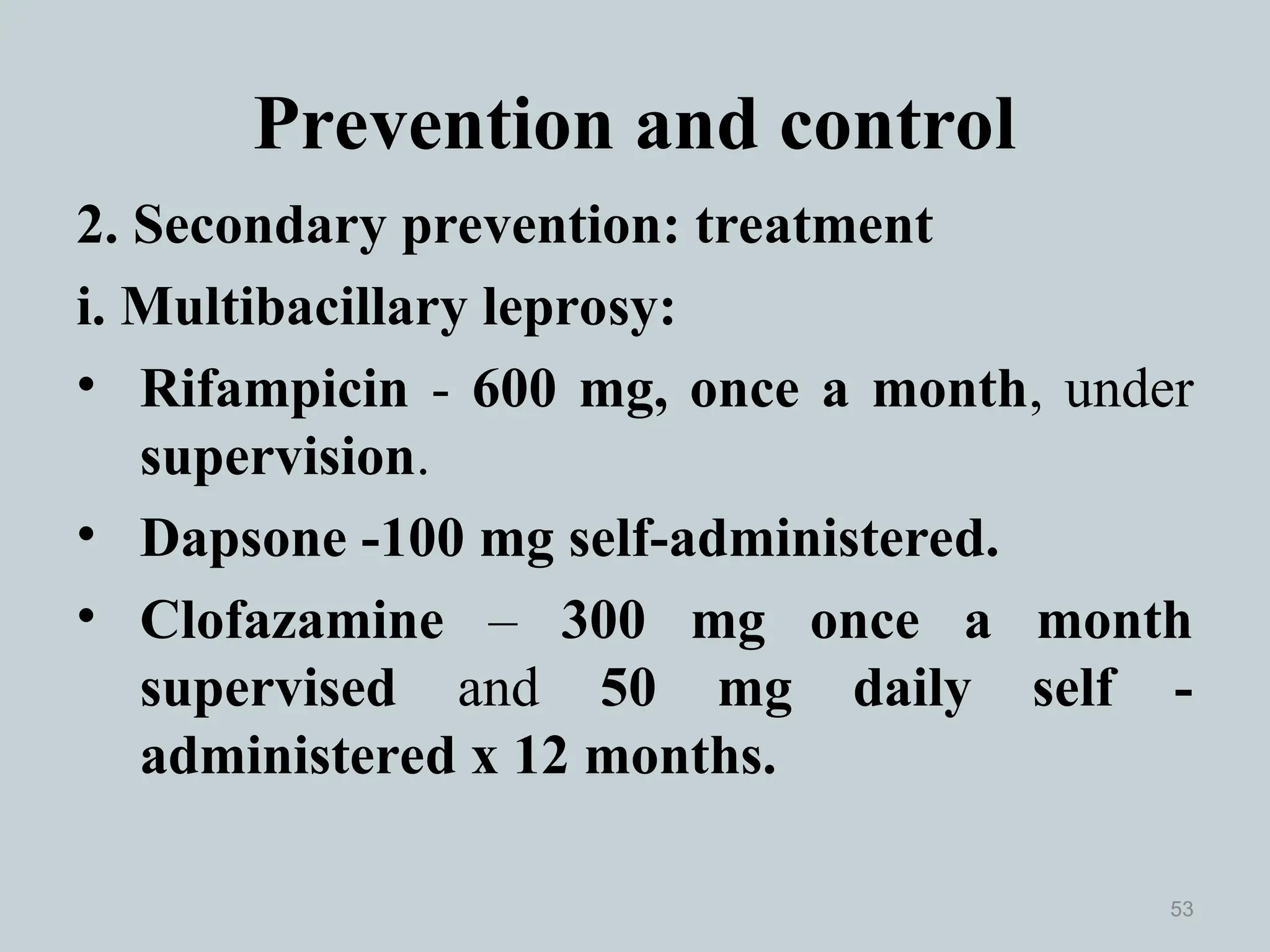
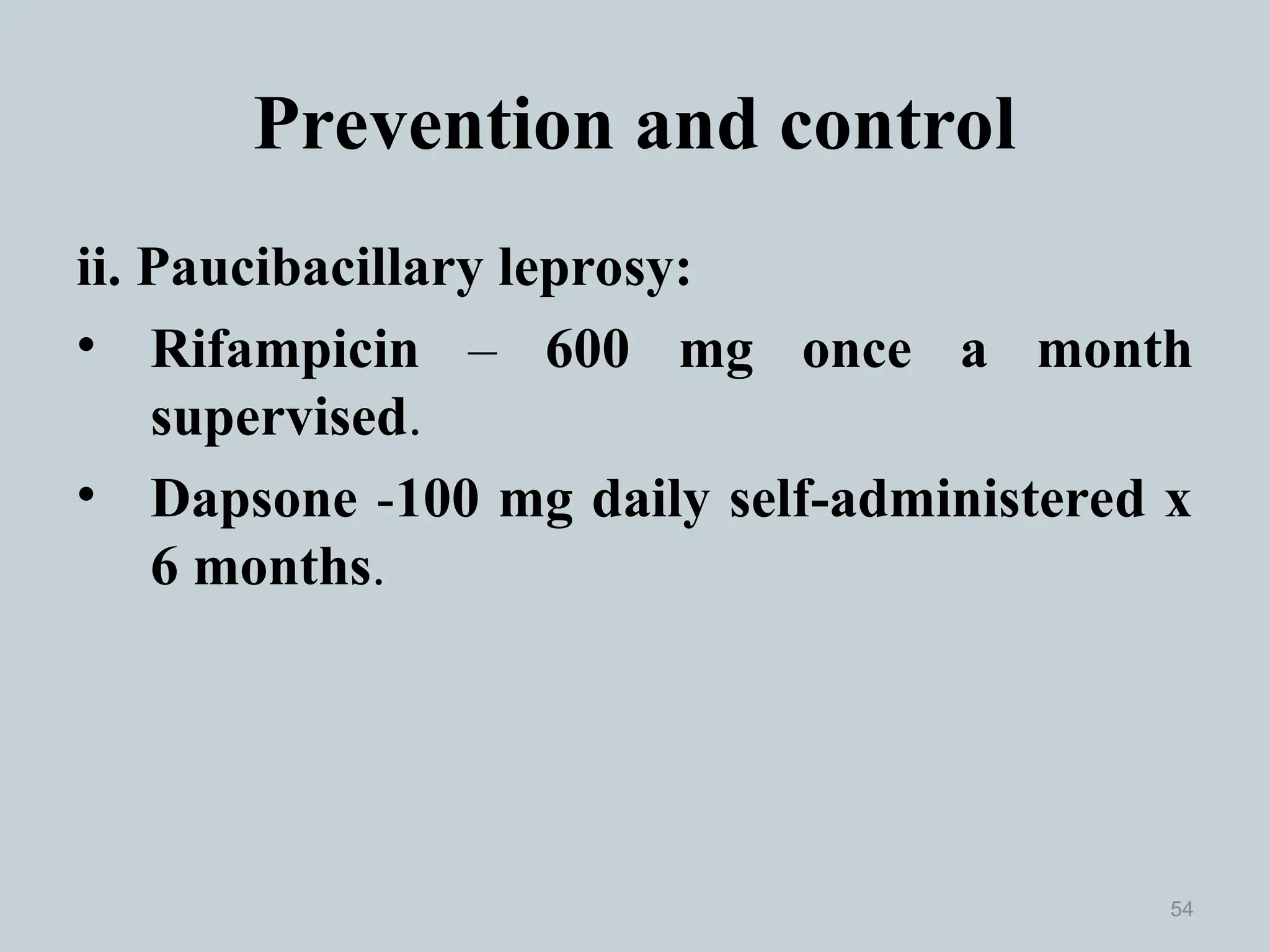
The document discusses the epidemiology, prevention, and control of tetanus and leprosy, outlining their characteristics, modes of transmission, and clinical features. Tetanus is caused by Clostridium tetani, while leprosy is caused by Mycobacterium leprae, both diseases are endemic in India, with substantial public health concerns as highlighted by their case statistics. It emphasizes primary, secondary, and tertiary prevention strategies, including vaccination and health education initiatives to combat these infections.