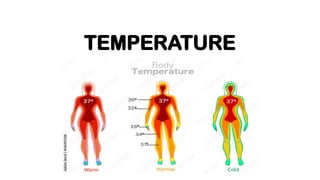
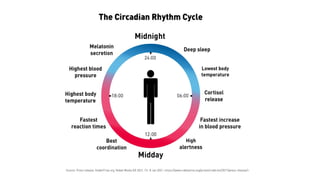
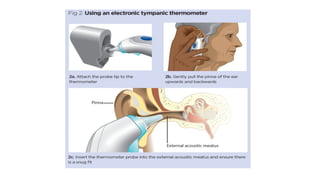
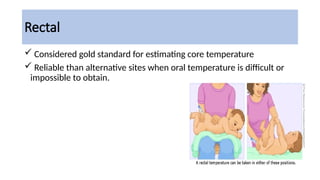
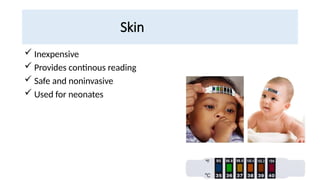
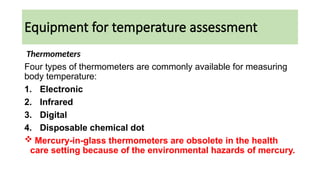
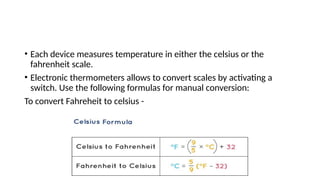
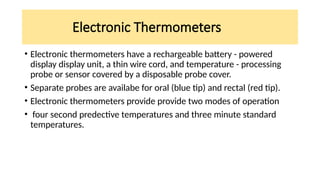
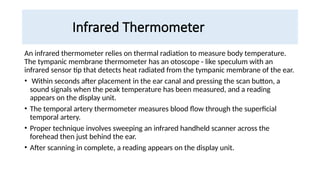
The document provides an overview of body temperature regulation, emphasizing the balance between heat production and loss, which is controlled mainly by the hypothalamus through physiological and behavioral mechanisms. It discusses factors affecting body temperature, including age, exercise, hormonal fluctuations, and environmental conditions, as well as methods for measuring temperature across different sites and devices. Additionally, it addresses the significance of temperature assessment in diagnosing health conditions and outlines the proper care for thermometers.