- The document discusses the use of telehealth in Southampton to monitor and treat patients with long term conditions like COPD, cardiac issues, diabetes, and more.
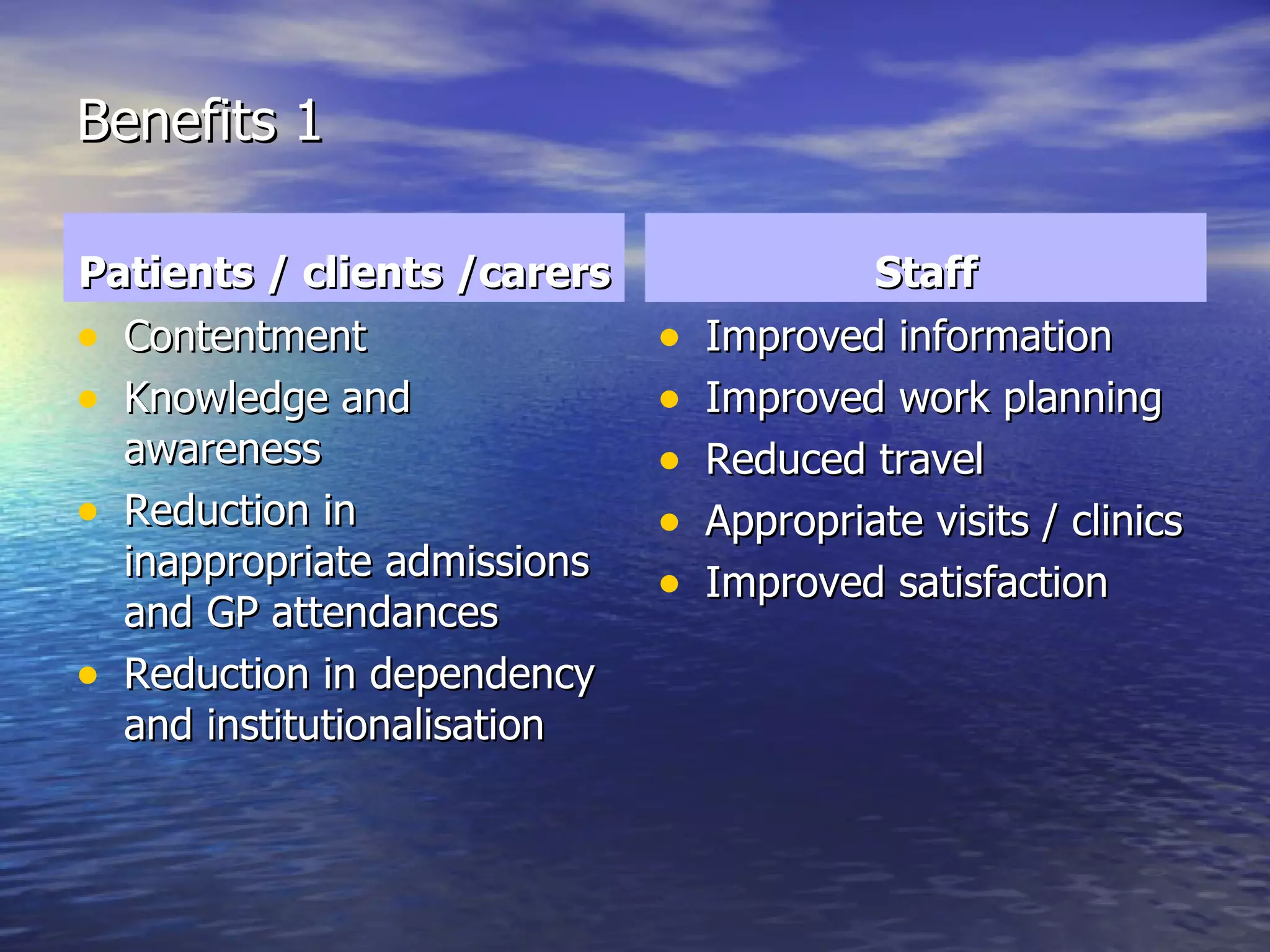
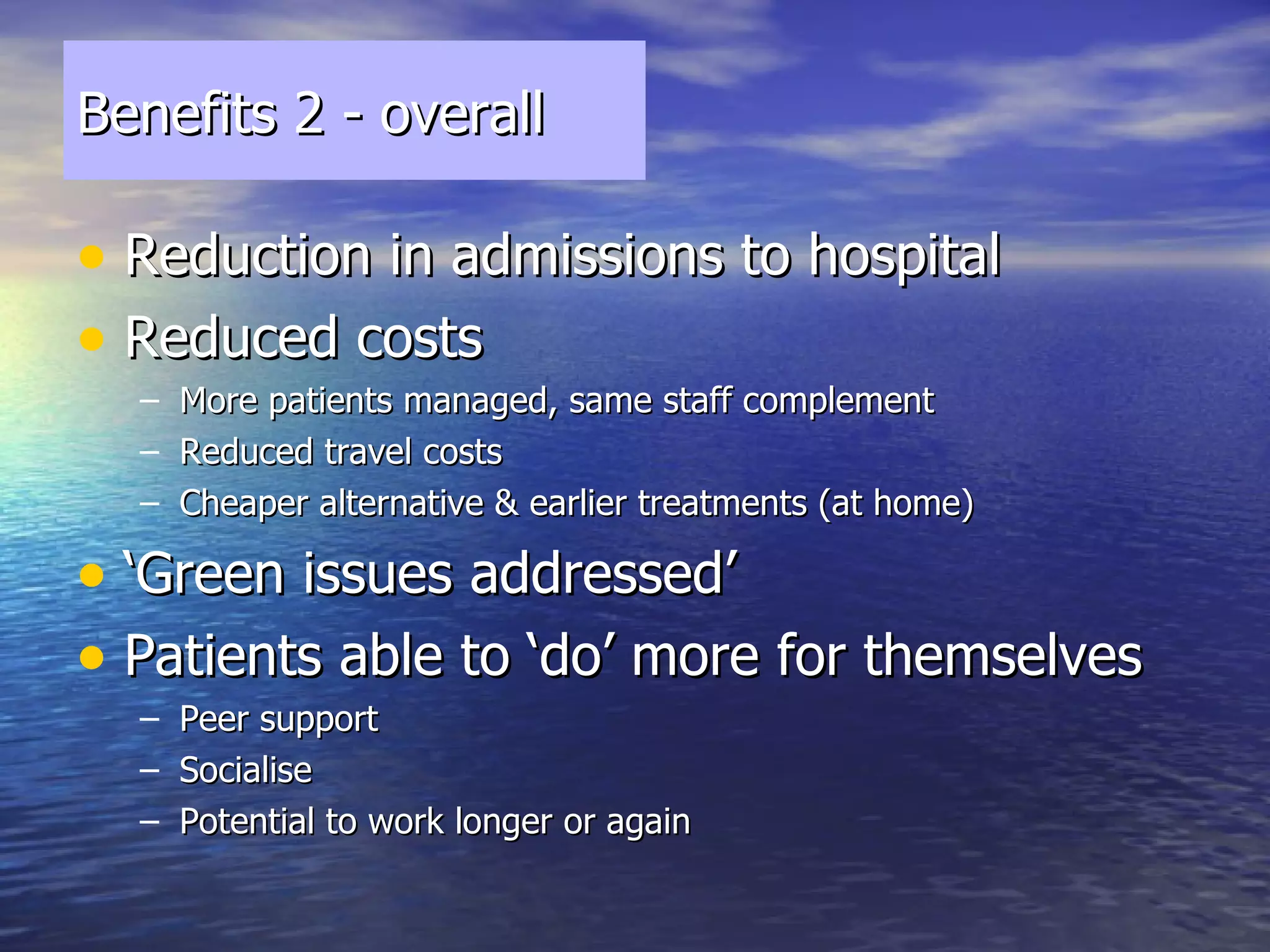
- Over 100 Docobo HealthHUB devices are used to remotely monitor patients' vital signs and symptoms. This has led to 242 avoided hospital admissions and improved outcomes for patients and the healthcare system.
- Barriers to expanding telehealth include finances, information governance challenges across organizations, and cultural resistance from staff. However, plans are in place to further integrate telehealth into clinical pathways and purchase more devices.