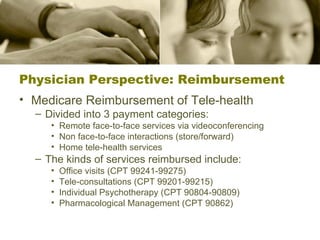
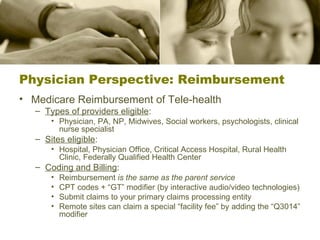
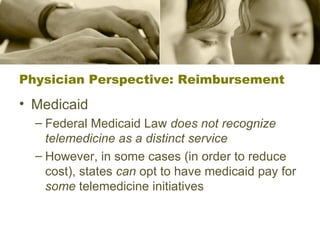
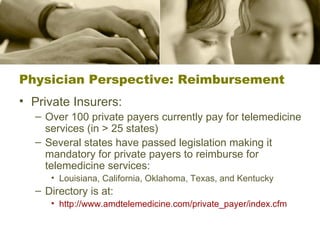
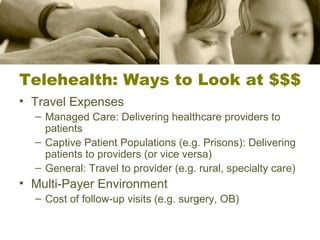
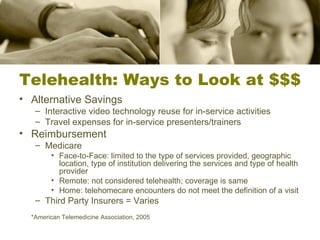
This document provides an overview of interactive health communication systems and telehealth technologies. It discusses physician perspectives on adoption barriers like workflow integration and reimbursement issues. It also profiles two AHRQ grants that utilize telehealth to improve cancer care in rural areas and provide remote monitoring for heart failure patients.





![Contact Information Brian Dixon, M.P.A. [email_address] (317) 554-0000 x4484 Atif Zafar, M.D. [email_address] (317) 554-0000 x2067 Julie McGowan, Ph.D., FACMI [email_address] (317) 274-7183](https://image.slidesharecdn.com/HealthCommunicationsSystems-123614464023-phpapp01/85/Health-Communications-Systems-29-320.jpg)