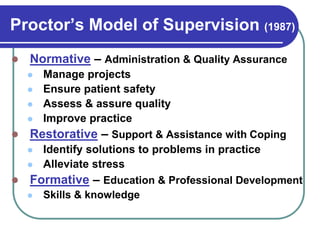
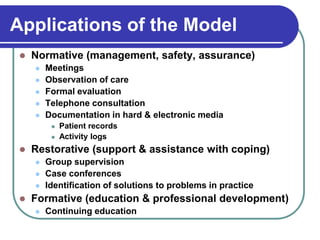
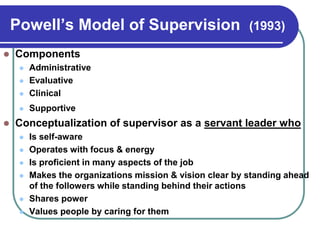
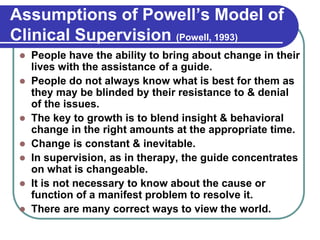
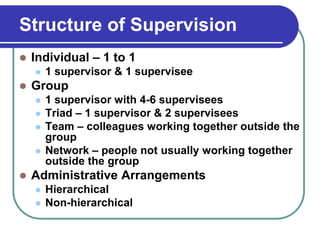
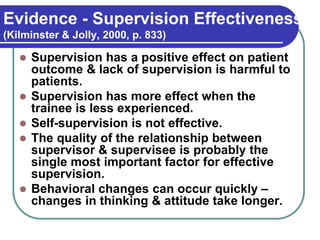
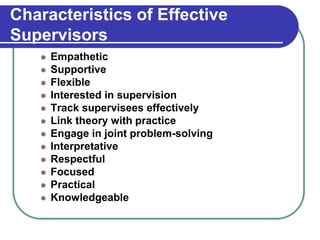
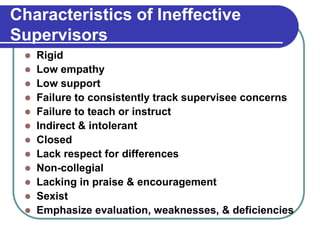
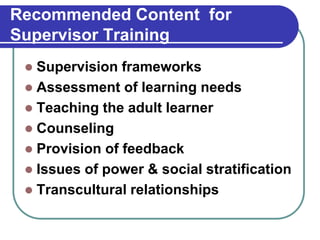
This document discusses frameworks and models for clinical supervision in healthcare. It describes Proctor's 1987 model of normative, restorative, and formative supervision. Heron's 1989 model includes authoritative and facilitative supervision interventions. Powell's 1993 model includes administrative, evaluative, clinical and supportive components. The document also discusses evidence that effective supervision improves patient outcomes, is most impactful for less experienced trainees, and depends most on the quality of the supervisor-supervisee relationship. Characteristics of effective supervisors include being empathetic, supportive, flexible and focused, while ineffective supervisors are rigid, lack empathy and support, and emphasize weaknesses.