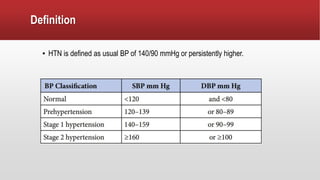
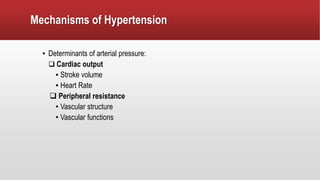
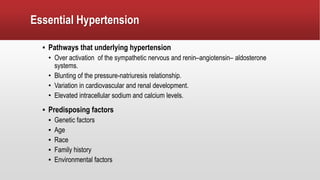
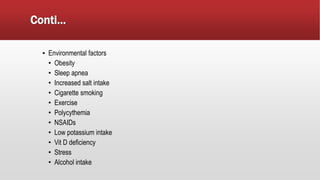
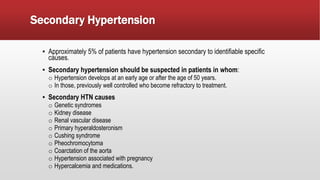
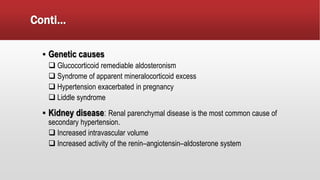
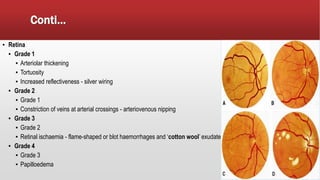
Systemic hypertension is defined as a usual blood pressure of 140/90 mmHg or higher. It doubles the risk of cardiovascular diseases and is a leading cause of death worldwide. There are two main types - primary/essential hypertension which accounts for 95% of cases and has no identifiable cause, and secondary hypertension which is caused by specific conditions like kidney disease or hormonal disorders. Untreated hypertension can lead to serious complications affecting the heart, brain, kidneys and eyes. Management involves identifying and treating any underlying causes, along with lifestyle modifications and medication to control blood pressure.