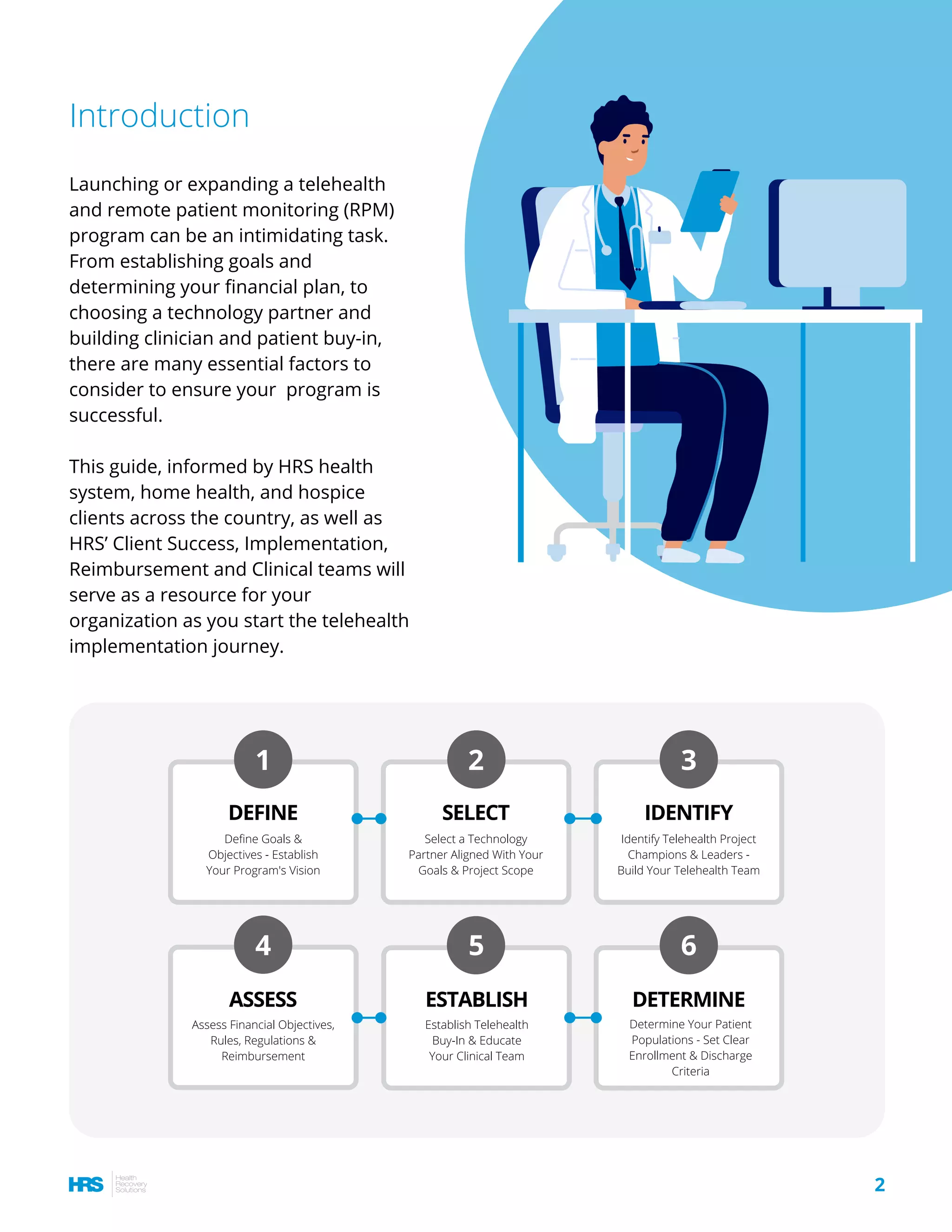
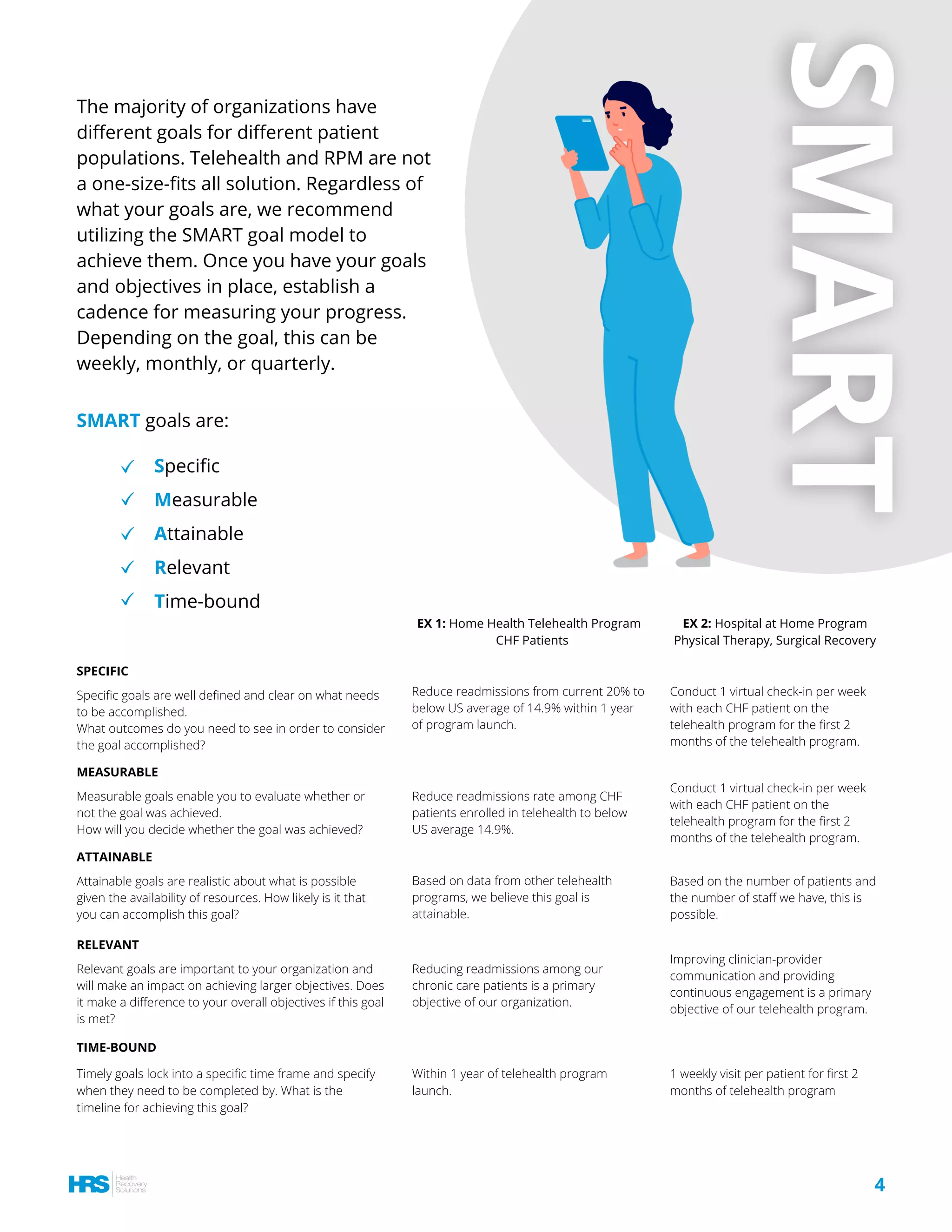
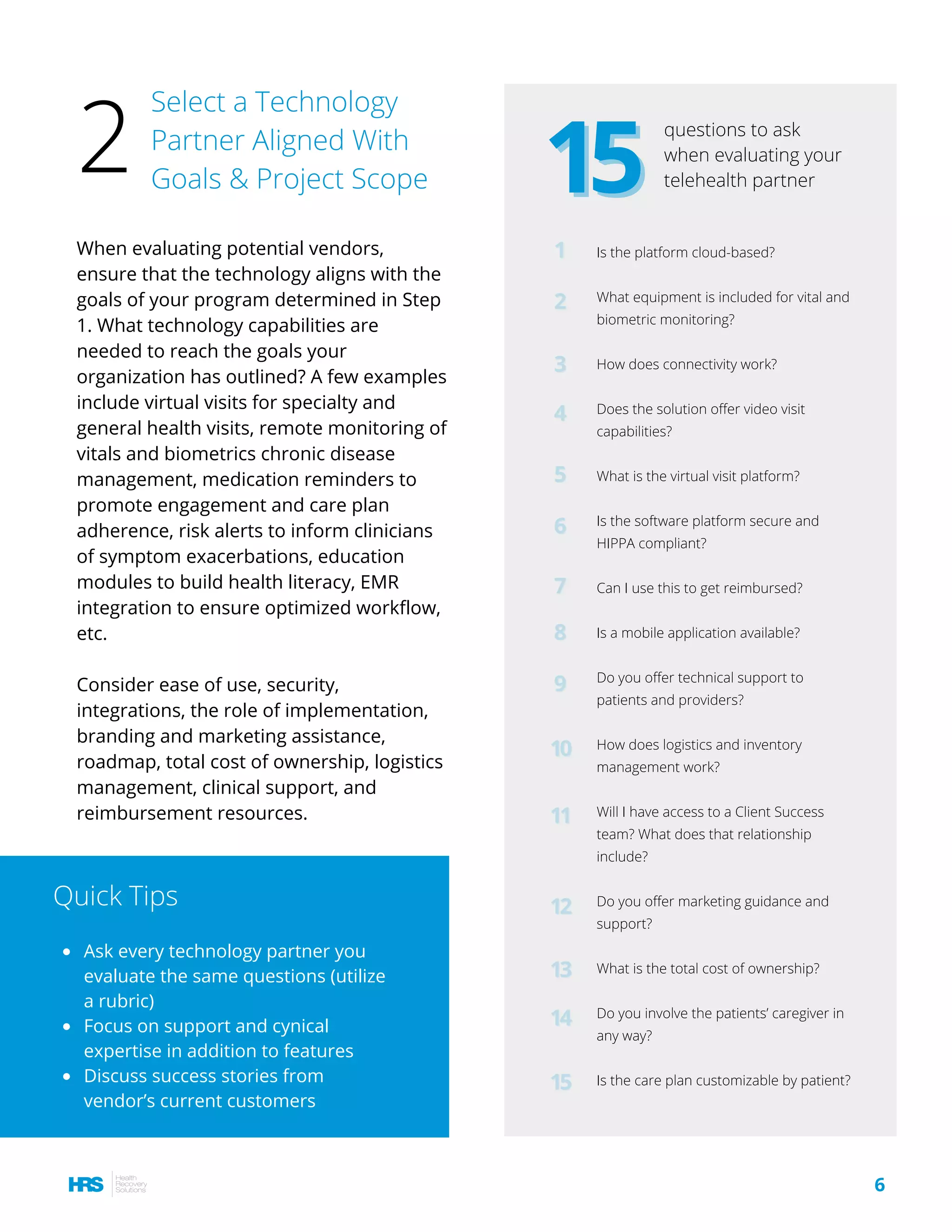
The document outlines six essential steps for establishing a successful telehealth and remote patient monitoring (RPM) program, including defining goals, selecting technology partners, identifying project champions, assessing financial objectives, and educating clinical teams. It emphasizes the importance of clear objectives, aligning goals with the organization's mission, and employing the SMART criteria for goal-setting. The guide also highlights the need for leadership roles to ensure effective program execution and the necessity of ongoing education and support for clinicians to maximize program utilization.