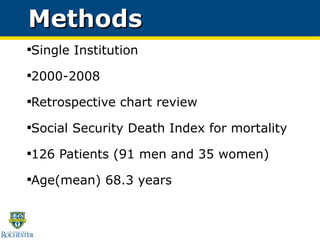
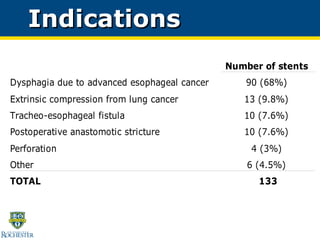
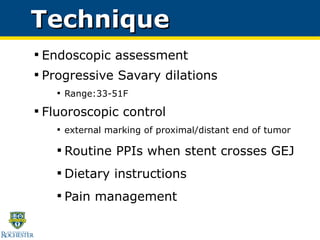
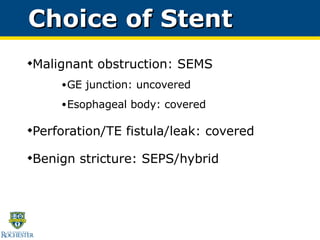
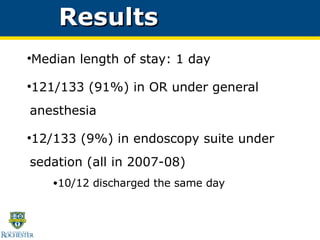
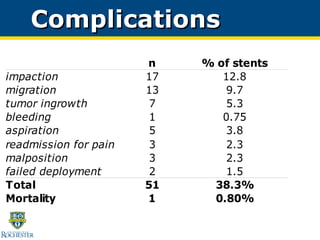
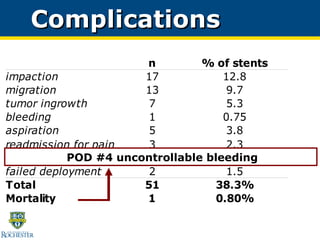
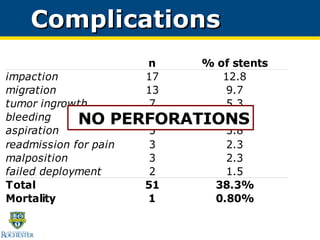
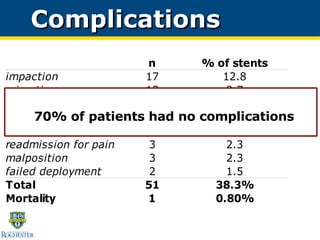
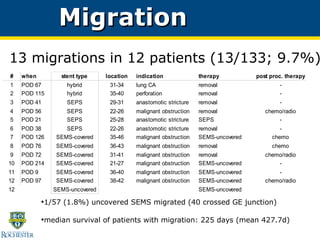
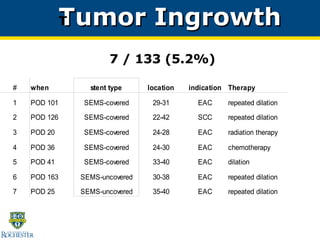
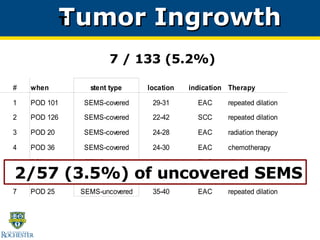
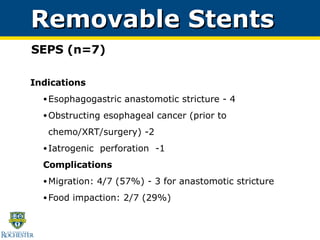
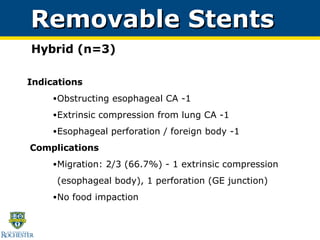
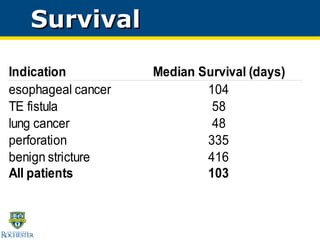
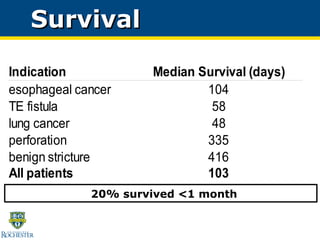
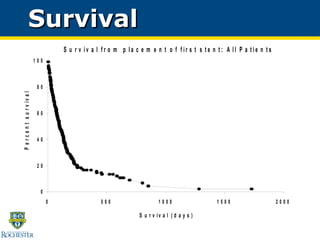
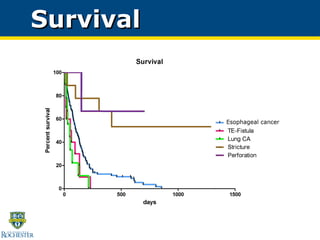
This study evaluated the use of self-expanding metal stents, plastic stents, and hybrid stents to treat 133 patients with malignant and benign esophageal diseases over an 8-year period at a single institution. Stent placement was successful in relieving obstruction in 91% of patients with a median hospital stay of 1 day. Complications included migration in 9.7% of cases, impaction in 13% requiring endoscopic disimpaction, and tumor ingrowth in 5.2% of uncovered metal stents. Stent placement was found to be a generally safe, quick, and reliable procedure for palliating malignant esophageal obstructions.