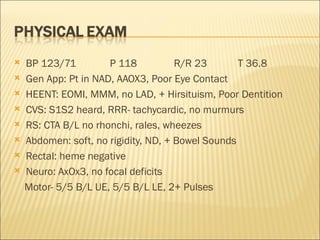
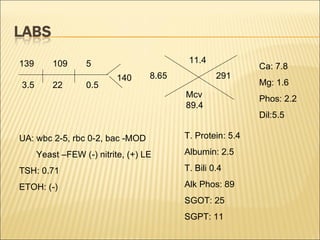
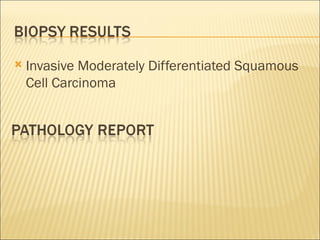
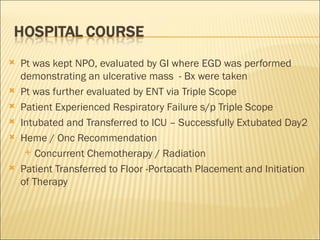
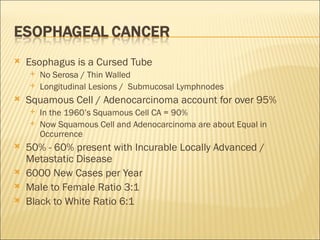
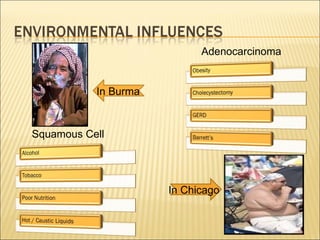
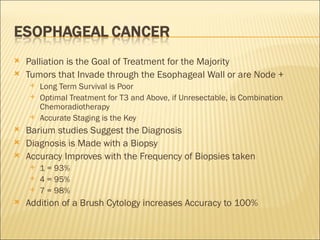
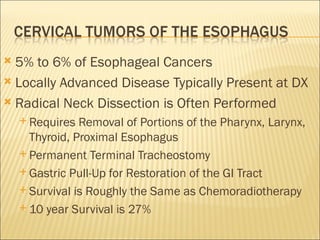
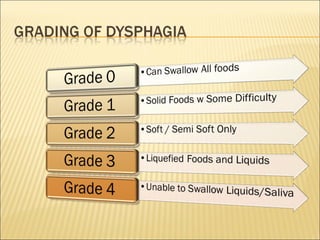
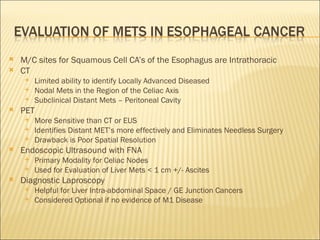
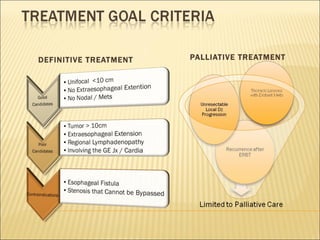
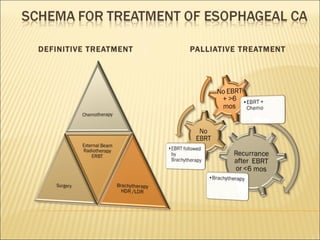
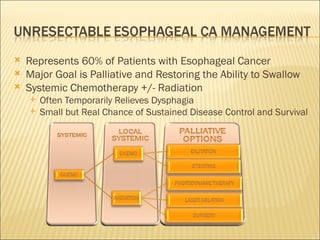
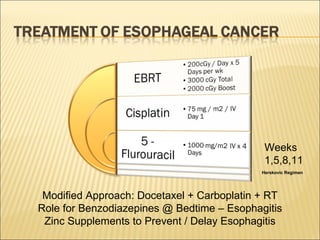
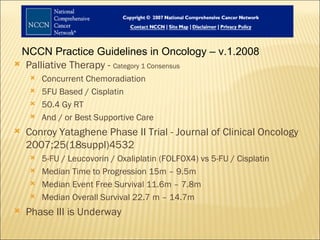
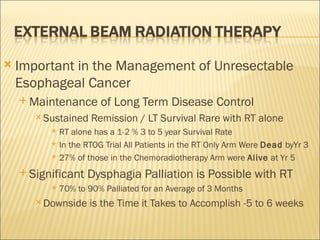
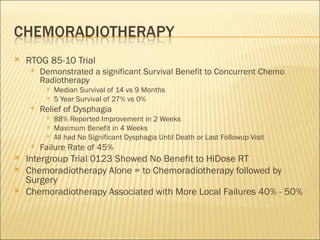
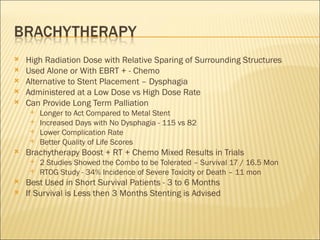
The patient is a 56-year-old African American female who presented with difficulty swallowing, weight loss, and weakness. An endoscopy revealed an ulcerative mass in the esophagus, and a biopsy showed moderately differentiated squamous cell carcinoma. She underwent chemotherapy and radiation therapy. Squamous cell carcinoma and adenocarcinoma account for over 95% of esophageal cancers. Definitive chemoradiation provides the best chance for local disease control and survival, with a 5-year survival rate of 27% compared to 0% for radiation alone. Palliative treatment aims to relieve dysphagia through methods like stenting or brachytherapy.