This case report describes a 26-year-old woman who experienced a spasm of the near reflex (accommodation, convergence, and miosis) when either eye was occluded or subjected to dioptric or non-dioptric blur. Her visual acuity decreased dramatically and an esodeviation was observed when either eye was occluded. Various occluders and lenses were able to trigger the spasm when a specific threshold of visual disruption was reached for each stimulus. Cycloplegia did not eliminate the spasm. This appears to be a rare case of a functional spasm of the near reflex triggered by binocular vision disruption, suggesting a potential anomaly in the neurological pathways involved in the

![triggered the spasm of the near reflex. This test was repeated several
times, and the same result was obtained each time.
Neutral-Density Filter Bar and Bagolini Red Filter
Bar (Sbisa Bar)
A neutral-density filter bar from 0.3 to 1.8 log unit optical
density values was placed in front of one eye over the glasses. The
spasm of the near reflex was induced when filter 0.9 (5.40 log of
luminance12
) and all darker filters were placed in front of the eye.
Filter number 10 (5.00 log of luminance12
) of the Bagolini red
filter bar induced the characteristic spasm, but not the lighter ones.
A normal sensory fusion response was reported with filter 9 (5.08
log of luminance12
), whereas filter 10 induced marked uncrossed
diplopia. Those neutral-density and red filters reduce the overall
luminance with only minimal visual acuity reduction (20/20 [6/6]
to 20/25 [6/7.5]).
For all the tested conditions, a spasm of the near reflex was
triggered whenever the left or the right eye was occluded. The
spasm was always immediately reversed when any of the occluders
inducing the spasm was removed. Cycloplegia (1 drop of cyclopen-
tolate HCl 1%) did not abolish this particular reaction to occlu-
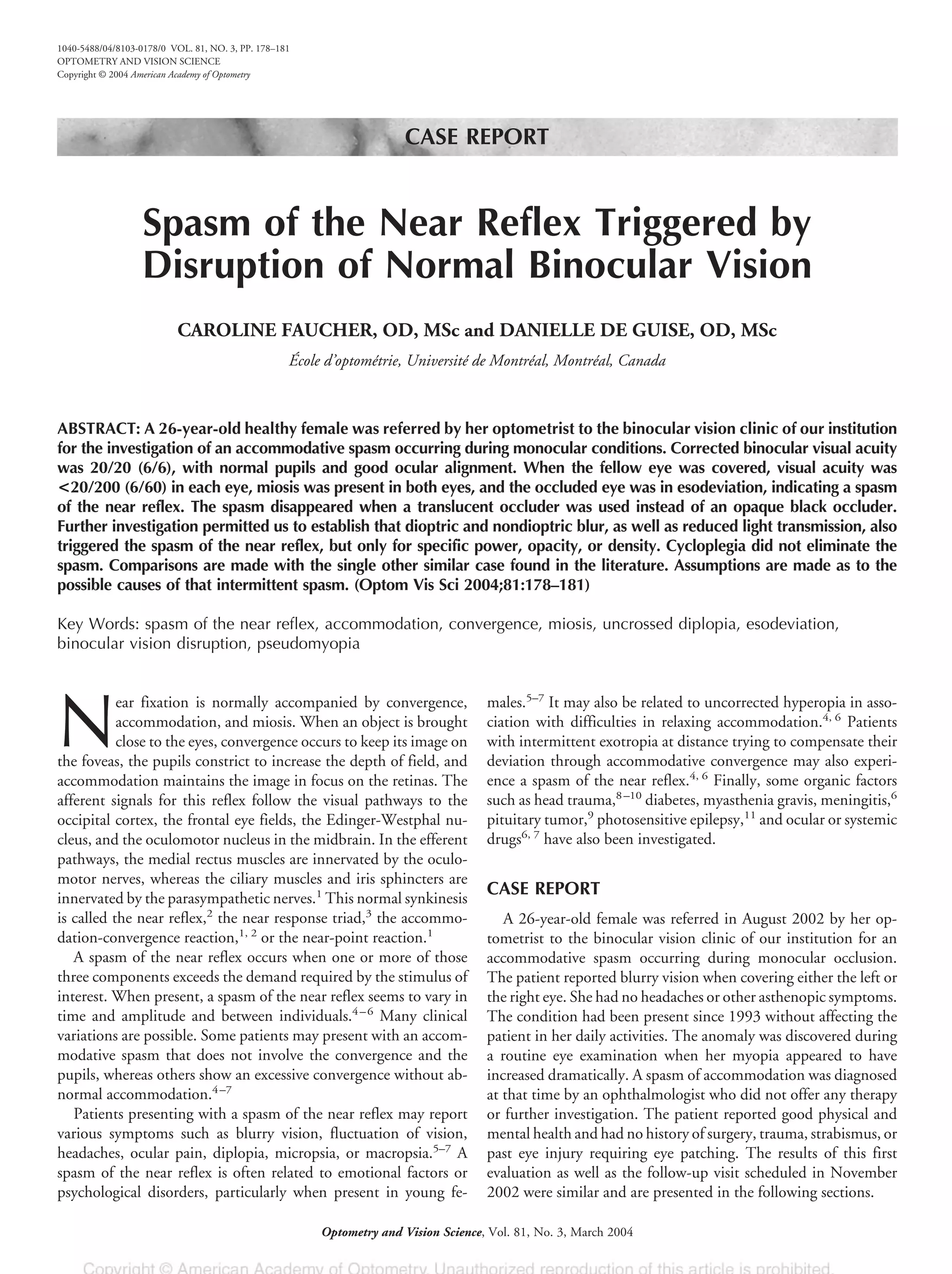
sion. Fig. 3 shows the patient with ϩ3.00 D (Fig. 3 A and C) and
ϩ3.50 D (Fig. 3 B and D) trial lenses, before cycloplegia (Fig. 3 A
and B) and during cycloplegia (Fig. 3 C and D). Note the bilateral
miosis (Fig. 3B) and esodeviation of the “covered” eye with ϩ3.50
D (Fig. 3 B and D) but not with ϩ3.00 D (Fig. 3 A and C), even
though the ϩ3.00 D lens decreases the visual acuity to about
20/200 (6/60). The cycloplegic refraction gave results similar to
the patient’s current ophthalmic correction.
Dilated slit lamp and fundus examinations were normal in both
eyes. A neurological evaluation was not recommended because the
condition was already present 10 years ago, the patient was asymp-
tomatic, and the spasm was only triggered by specific viewing
conditions.
DISCUSSION
We reported the special case of a 26-year-old woman presenting
with an occlusion-induced spasm of the near reflex. To our knowl-
edge, only one similar case has been reported in the literature.
Rutstein and Marsh-Tootle4
presented the results from the clinical
evaluation of a 27-year-old female with an accommodative spasm
induced by the occlusion of her right eye only. Their clinical find-
ings, however, differ from ours in several ways. The spasm they
reported was not accompanied by an esodeviation, and the pupils
appeared to constrict only minimally. In their report, the dioptric
blur created by a ϩ5.00 D lens did not induce the spasm of the
near reflex. They did not investigate other forms of occlusion to
elicit the spasm reported. Furthermore, cycloplegia abolished the
accommodative spasm found in their patient, whereas in the
present case, marked convergence occurred even during cyclople-
gia. The differences observed between the two cases reported may
be explained by the fact that the one reported by Rutstein and
Marsh-Tootle showed only an accommodative spasm without any
associated excess of convergence. The authors speculated that the
phenomenon could be similar to latent nystagmus in that it occurs
only when one eye is covered. They mentioned that this could also be
related to the work of their patient as a photographer, suggesting a
possiblelinkwithinstrumentmyopia.Thislatterexplanationmaynot
be applicable to our patient because she does not need to close either
eyeforherworkorhobbiesandsheneverusesamicroscope,telescope,
or any other device requiring monocular vision.
This unusual case of binocular spasm of the near reflex during
monocular occlusion without any associated history of ocular or
systemic disease or trauma is difficult to explain. The various stim-
uli used in our evaluation to disrupt the binocular vision through
different degrees and mechanisms were able to induce a spasm of
the near reflex: total occlusion, dioptric and nondioptric blur with
visual acuity disturbance, and luminance attenuation without sig-
nificant visual acuity reduction. It is interesting to note that it was
possible to determine a threshold at which each of those conflicting
stimuli disturbed the binocular vision, even though these thresh-
olds could vary between visits. The spasm was triggered whenever
the left or the right eye received a threshold signal of sufficient
attenuation. When both eyes were opened and nothing interfered
with binocular vision, the eyes remained straight, the pupils were
normal, and the patient had no symptoms. This led us to conclude
FIGURE 3.
Dioptric blur with a ϩ3.00 D lens (A) does not induce the spasm, whereas
(B) it does with a ϩ3.50 D lens. The spasm is also triggered during
cycloplegia (D) with the ϩ3.50 D lens but (C) not with the ϩ3.00 D lens.
180 Spasm of the Near Reflex—Faucher & de Guise
Optometry and Vision Science, Vol. 81, No. 3, March 2004](https://image.slidesharecdn.com/spasmofthenearreflextriggeredbydisruption-140614181032-phpapp02/75/Spasm-of-the_near_reflex_triggered_by_disruption-9-3-2048.jpg)
