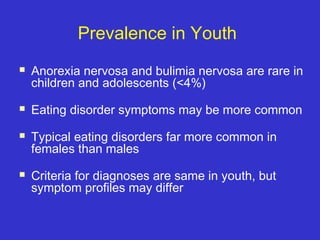
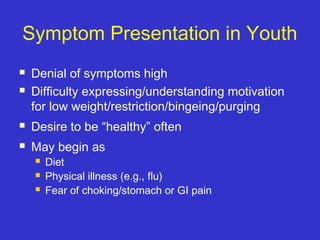
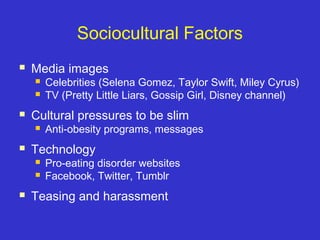
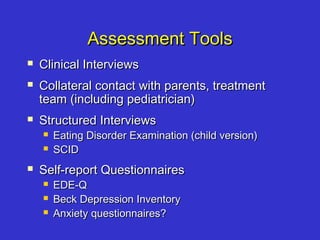
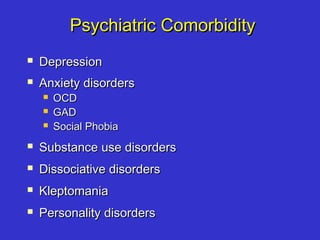
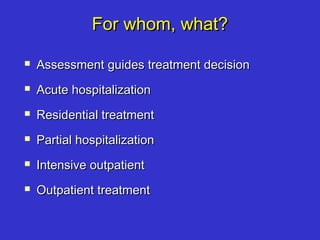
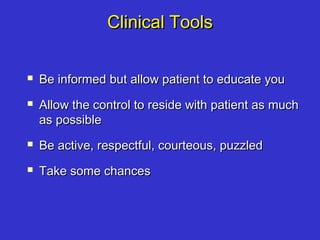
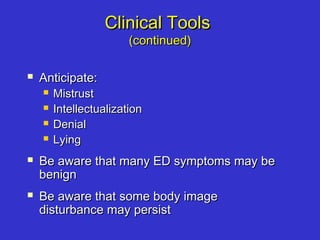
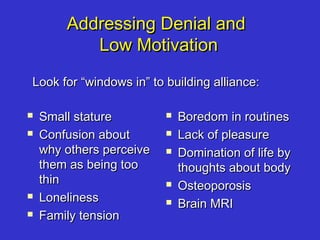
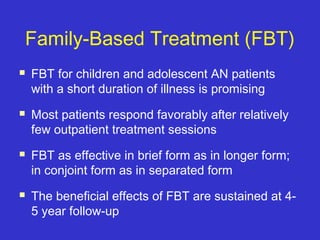
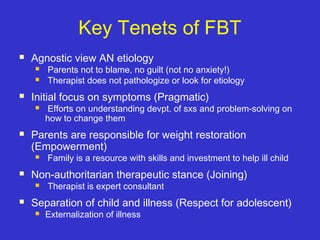
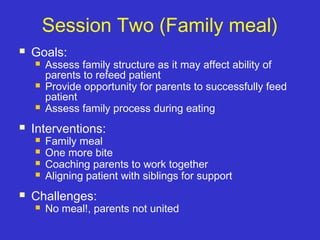
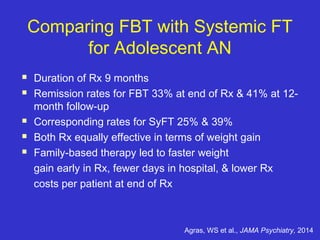
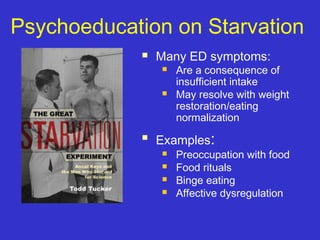
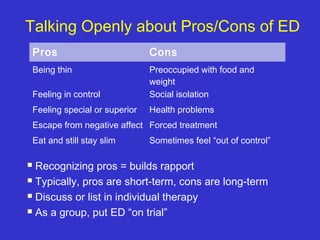
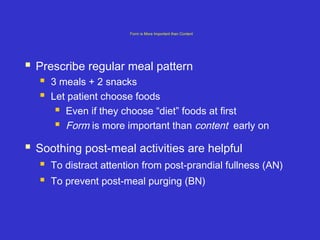
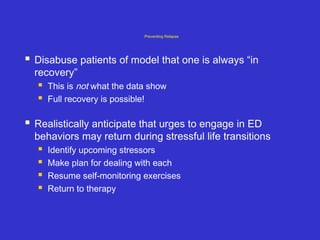
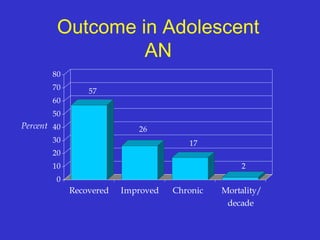
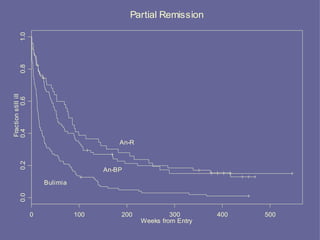
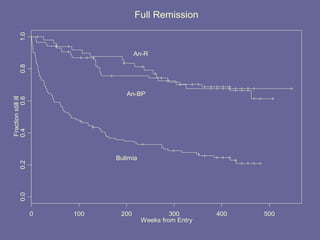
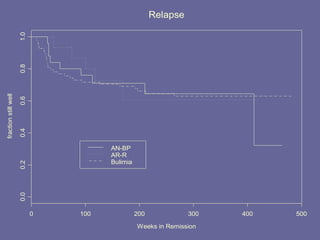
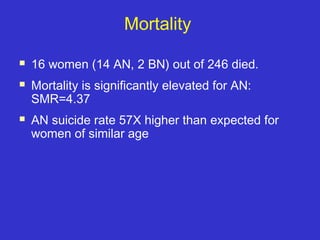
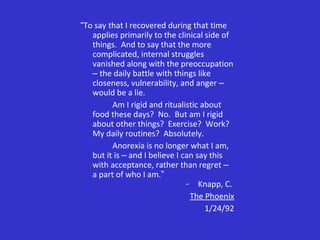
The document discusses the prevalence, symptom presentation, and treatment options for adolescents with eating disorders such as anorexia and bulimia. It highlights the importance of family-based treatment and cognitive behavioral therapy, addressing both clinical and psychological aspects of these disorders. Additionally, it outlines the long-term outcomes and challenges faced by individuals recovering from eating disorders.