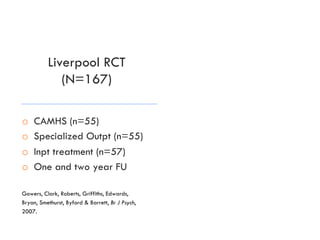
FBT is the most effective treatment for adolescent anorexia nervosa based on evidence from multiple randomized controlled trials:
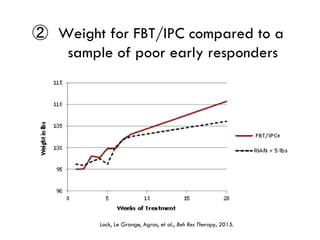
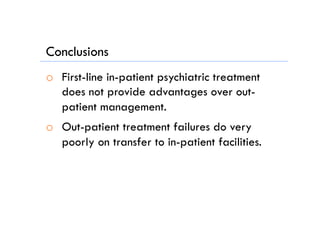
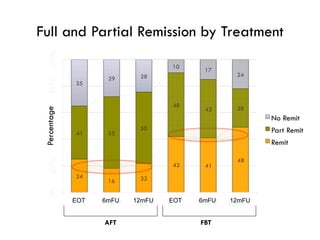
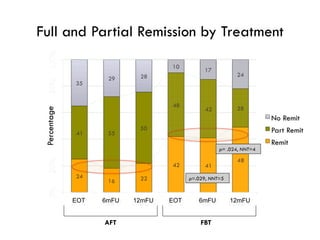
1) FBT leads to faster weight gain and symptom improvement compared to alternative therapies like adolescent focused therapy.
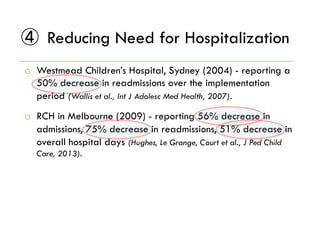
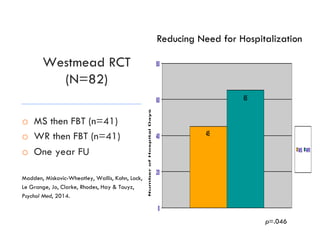
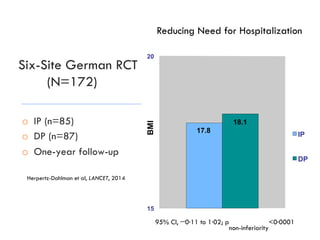
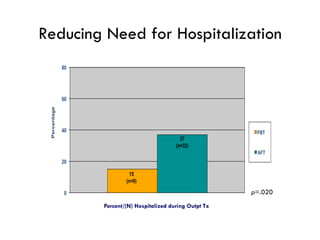
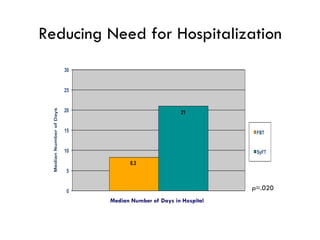
2) FBT reduces the need for hospitalization more than alternatives.
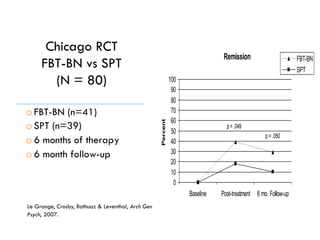
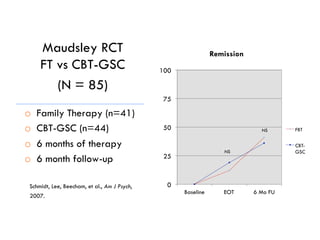
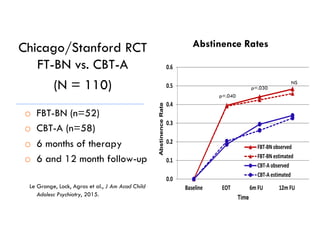
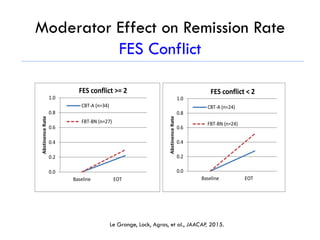
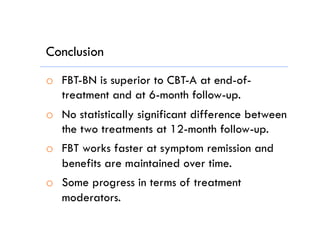
3) For bulimia nervosa, FBT and family therapy may lead to better outcomes than individual therapies like CBT at post-treatment and follow-up, though alternatives can also be effective.
![Weight gain >2 kgs. by wk 4 correctly characterized:
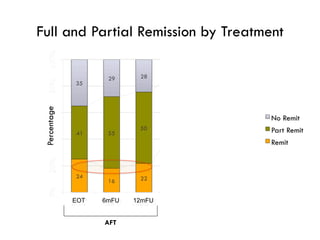
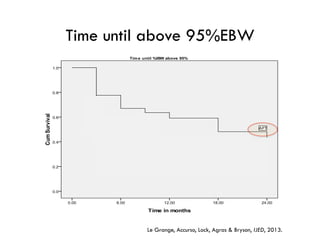
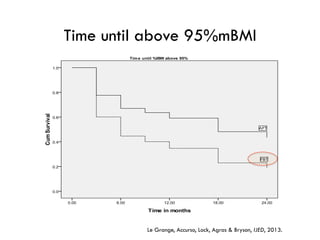
① Early Weight Gain and Outcome
(N>400 in FBT and AFT)
o 79% of responders [AUC = .814 (p<.001)]
o 71% of non-responders [AUC = .811 (p<.001)]
Doyle, Le Grange, Celio-Doyle, Loeb & Crosby, IJED, 2009; Le Grange, Accurso, Lock, Agras & Bryson, IJED, 2013;
Lock et al., JAACAP, 2005; Madden et al., IJED, 2015.](https://image.slidesharecdn.com/legrangecapgr2-160311183540/85/Le-grange-cap-gr-2-9-16-41-320.jpg)