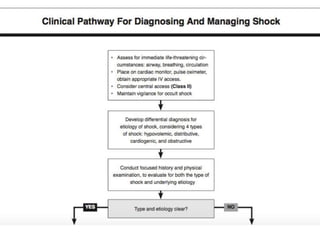
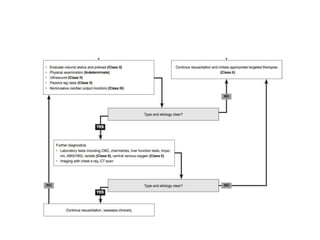
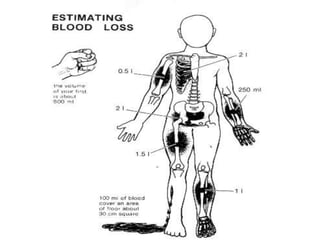
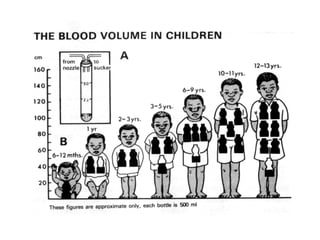
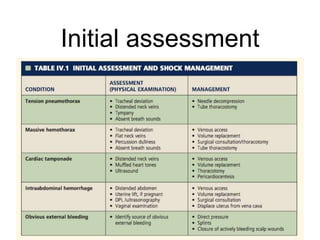
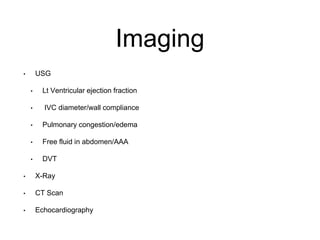
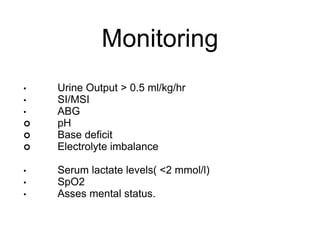
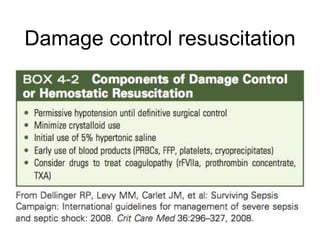
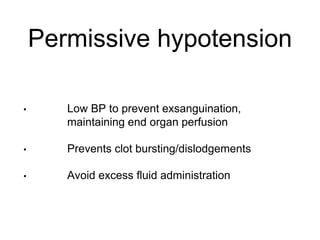
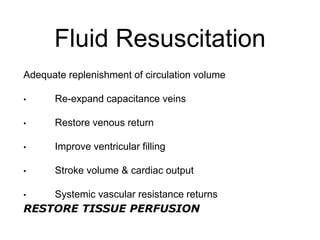
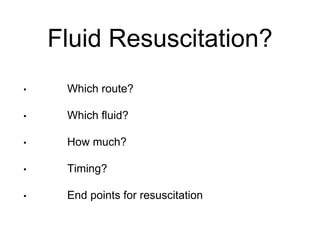
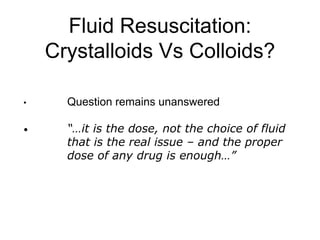
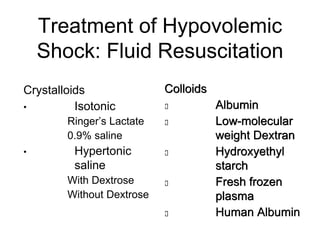
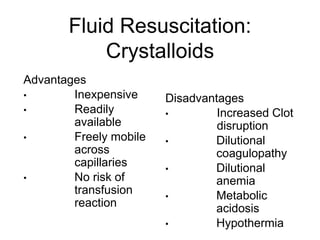
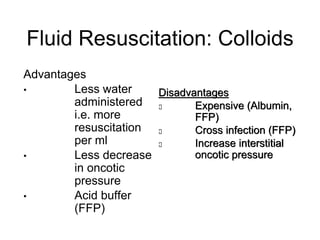
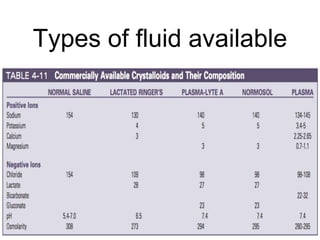
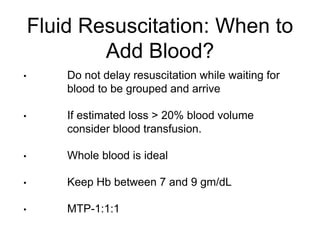
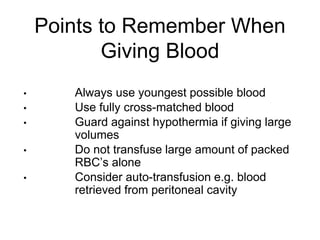
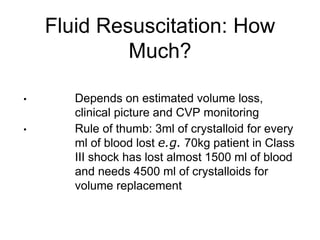
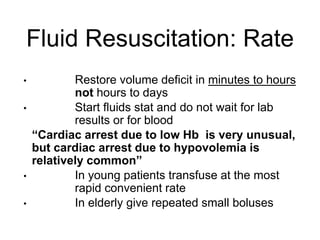
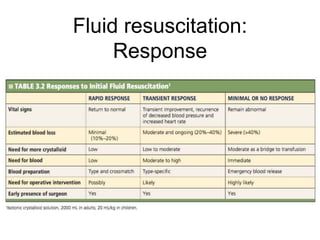
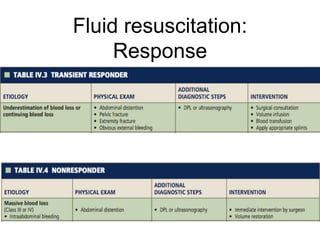
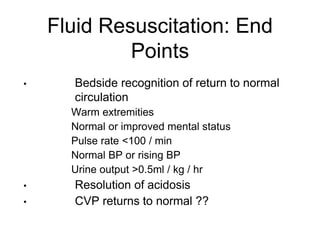
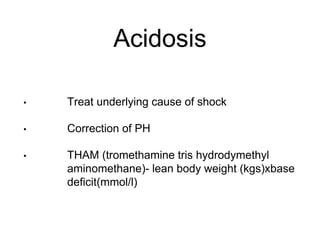
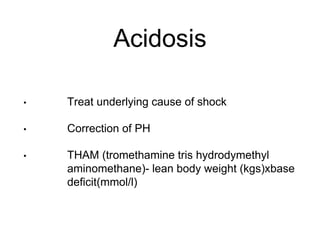
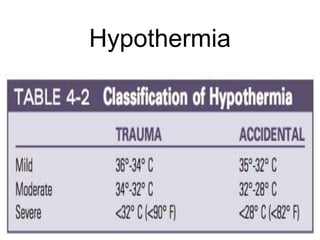
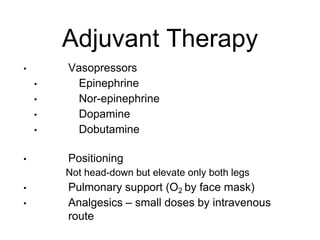
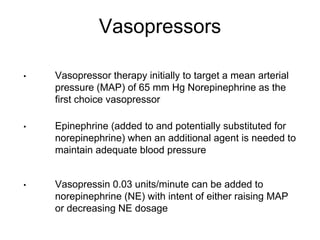
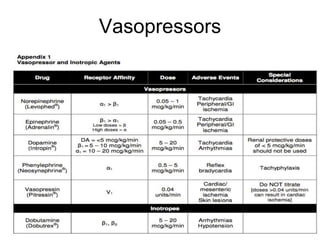
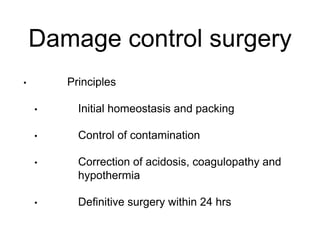
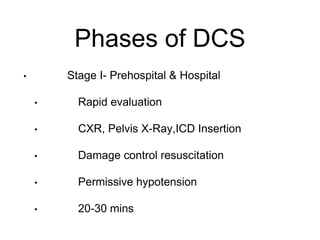
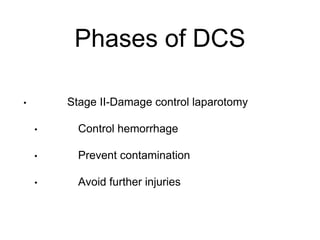
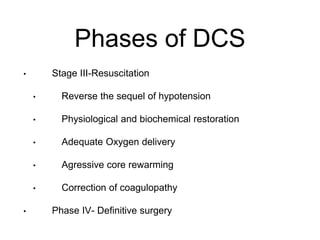
This document discusses the evaluation and management of shock. It begins by listing common clinical features of shock such as hypotension, tachycardia, and reduced urine output. The diagnosis of shock can be easy if there is overt volume loss or hemodynamic instability, but more challenging if loss is occult or slow. General management of shock includes ABCs, IV access, oxygen therapy, controlling fluid loss, and monitoring for things like urine output and lactate levels. Fluid resuscitation is important to replenish circulation volume using crystalloids or colloids. Goals of resuscitation are to restore tissue perfusion while avoiding complications like acidosis, hypothermia, and coagulopathy.