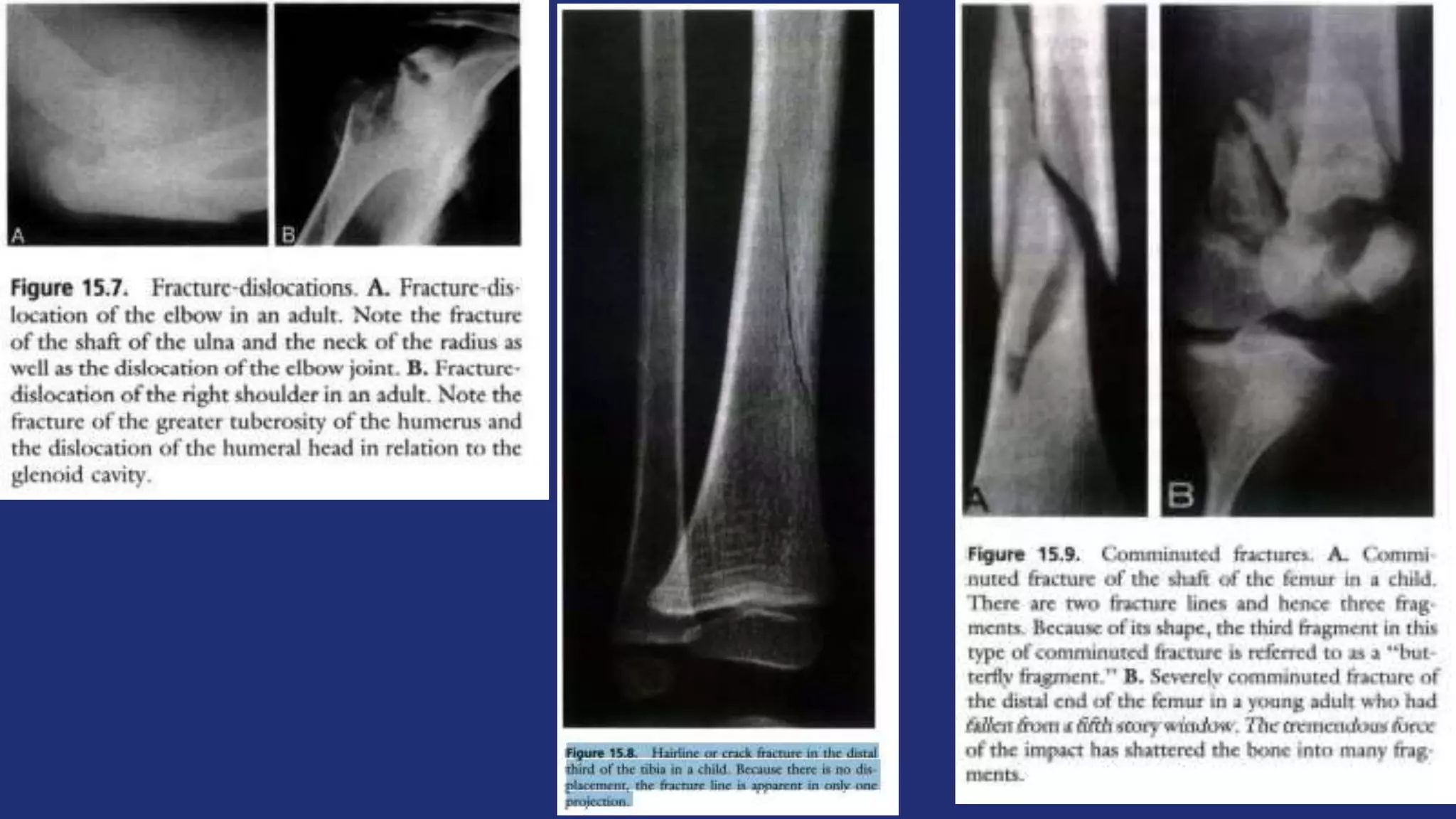
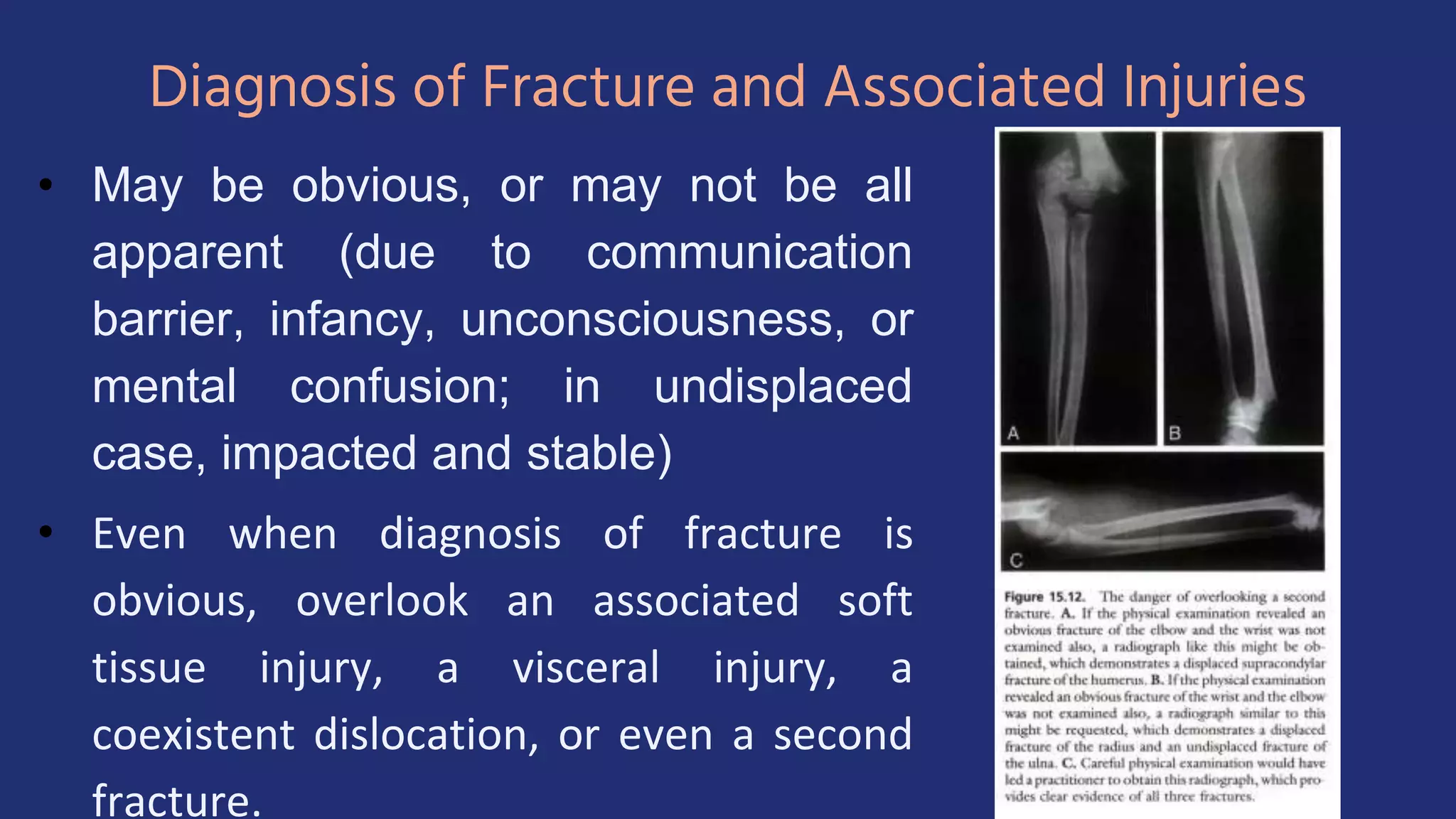
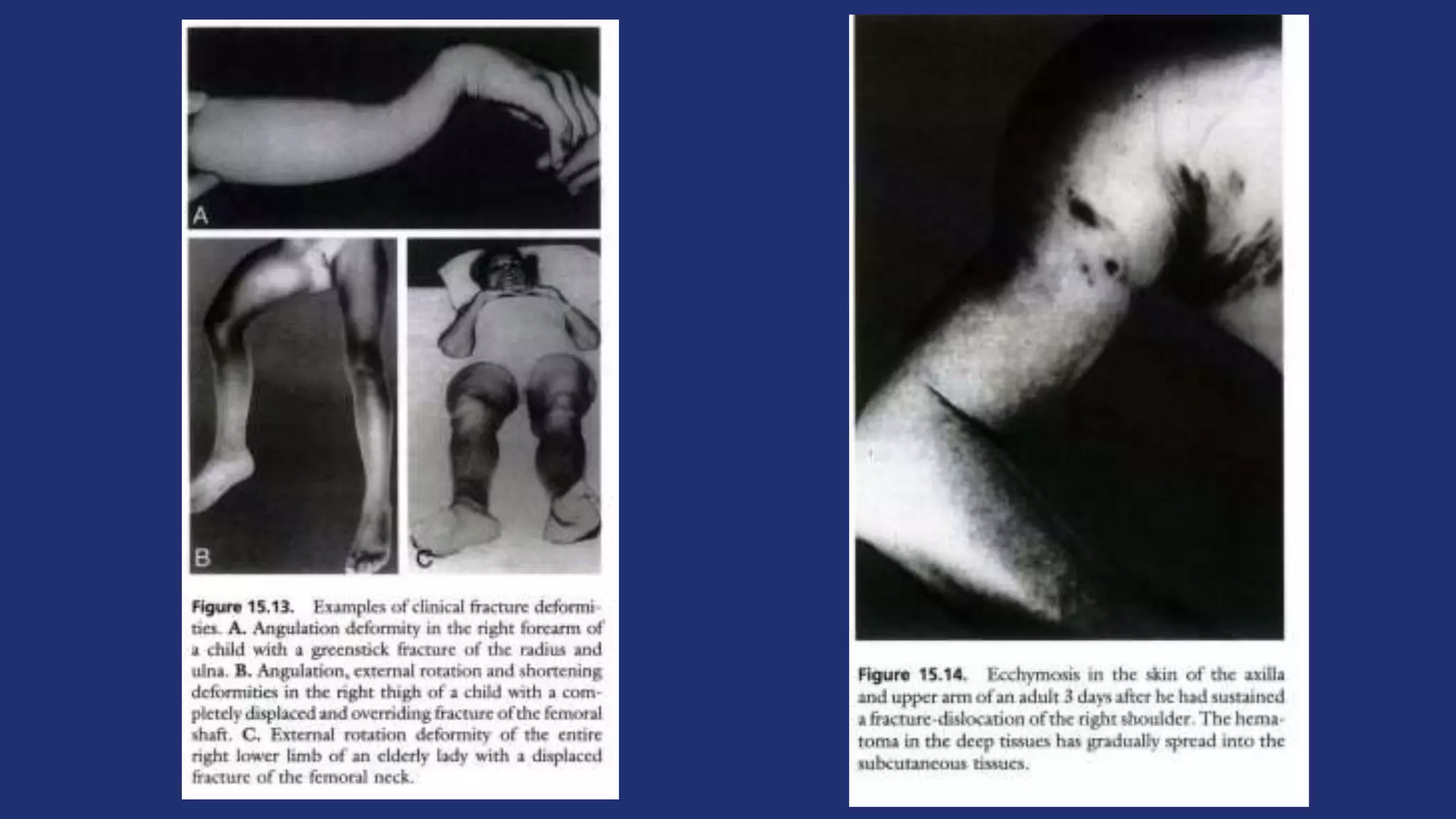
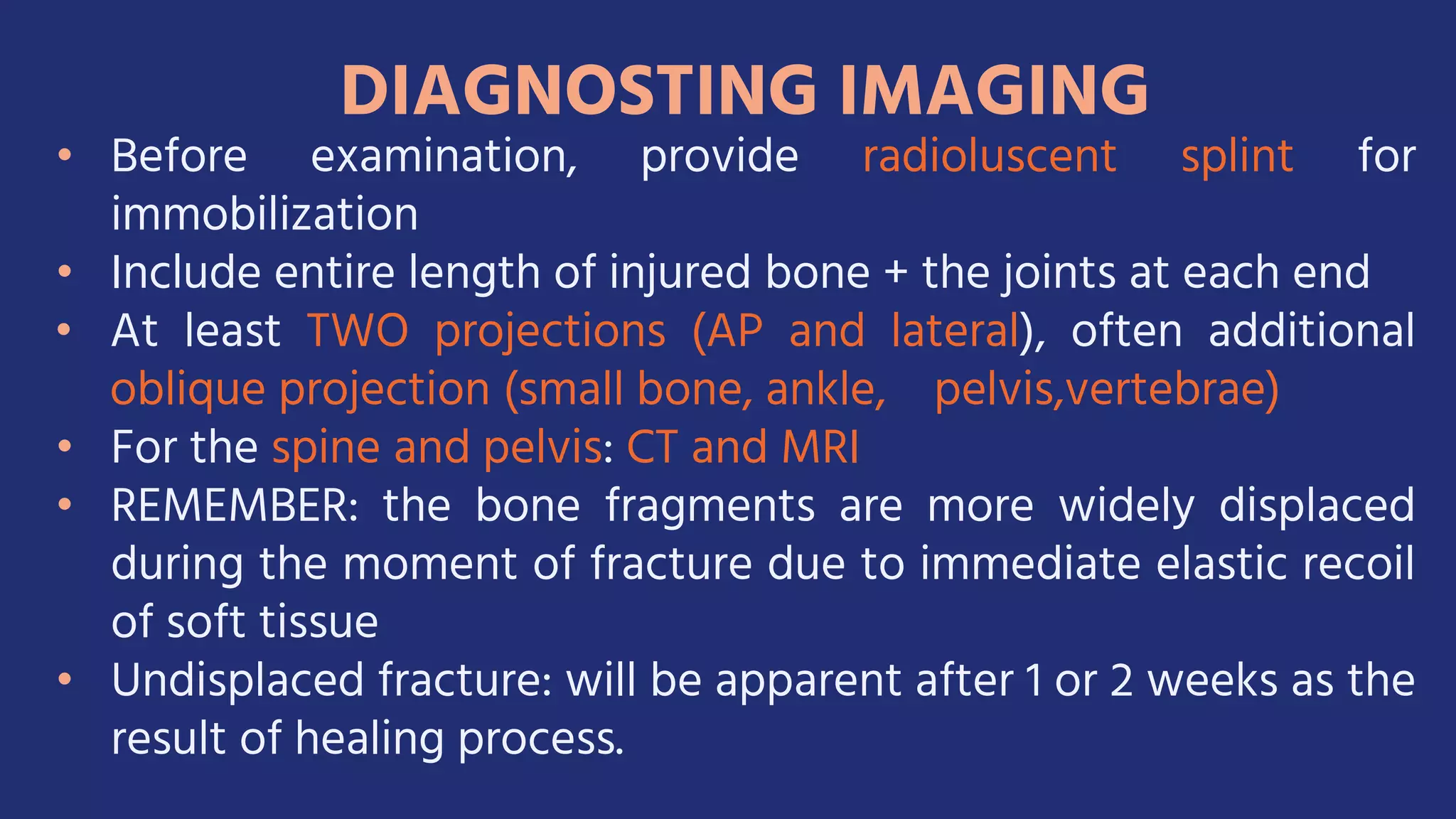
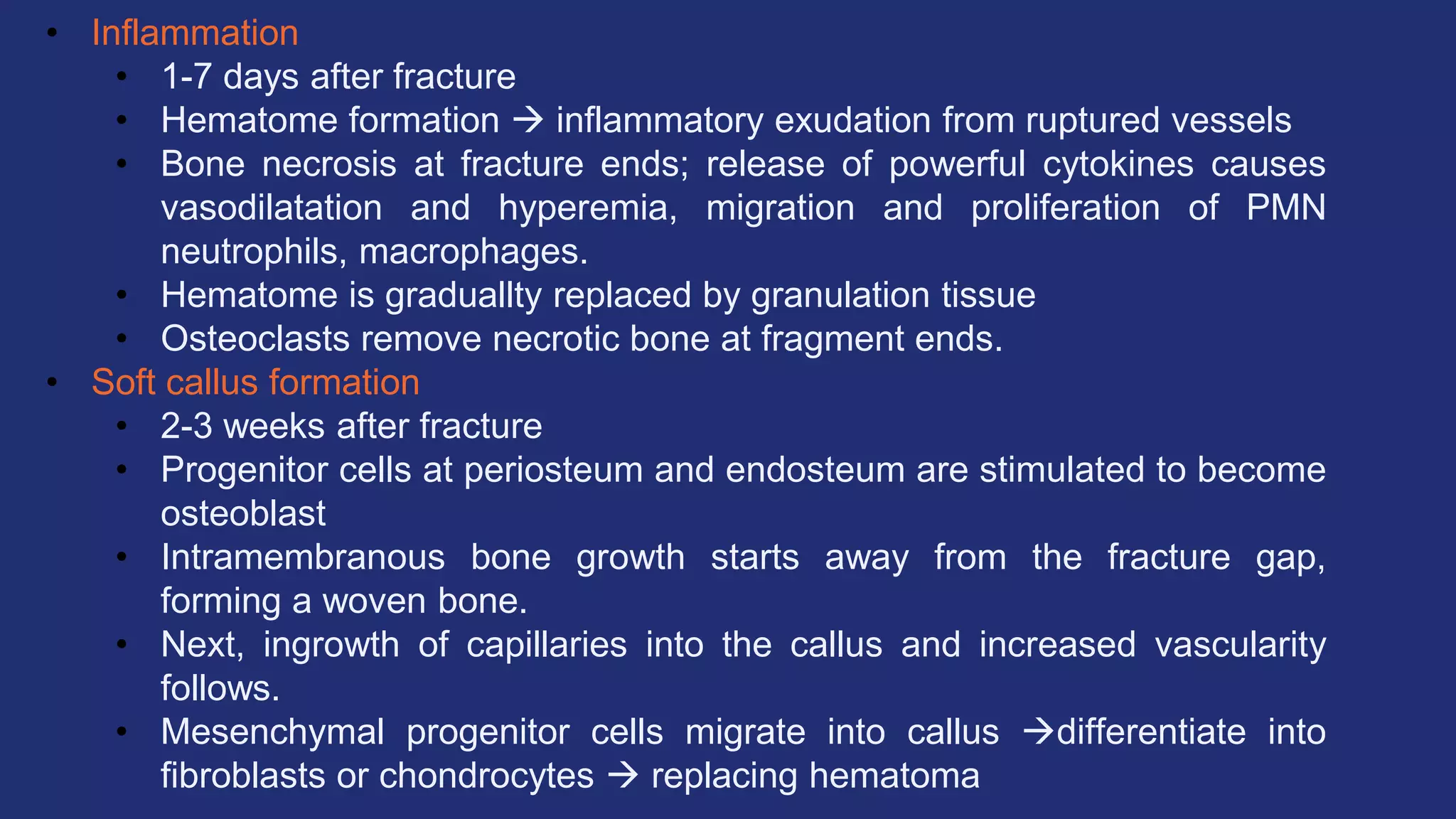
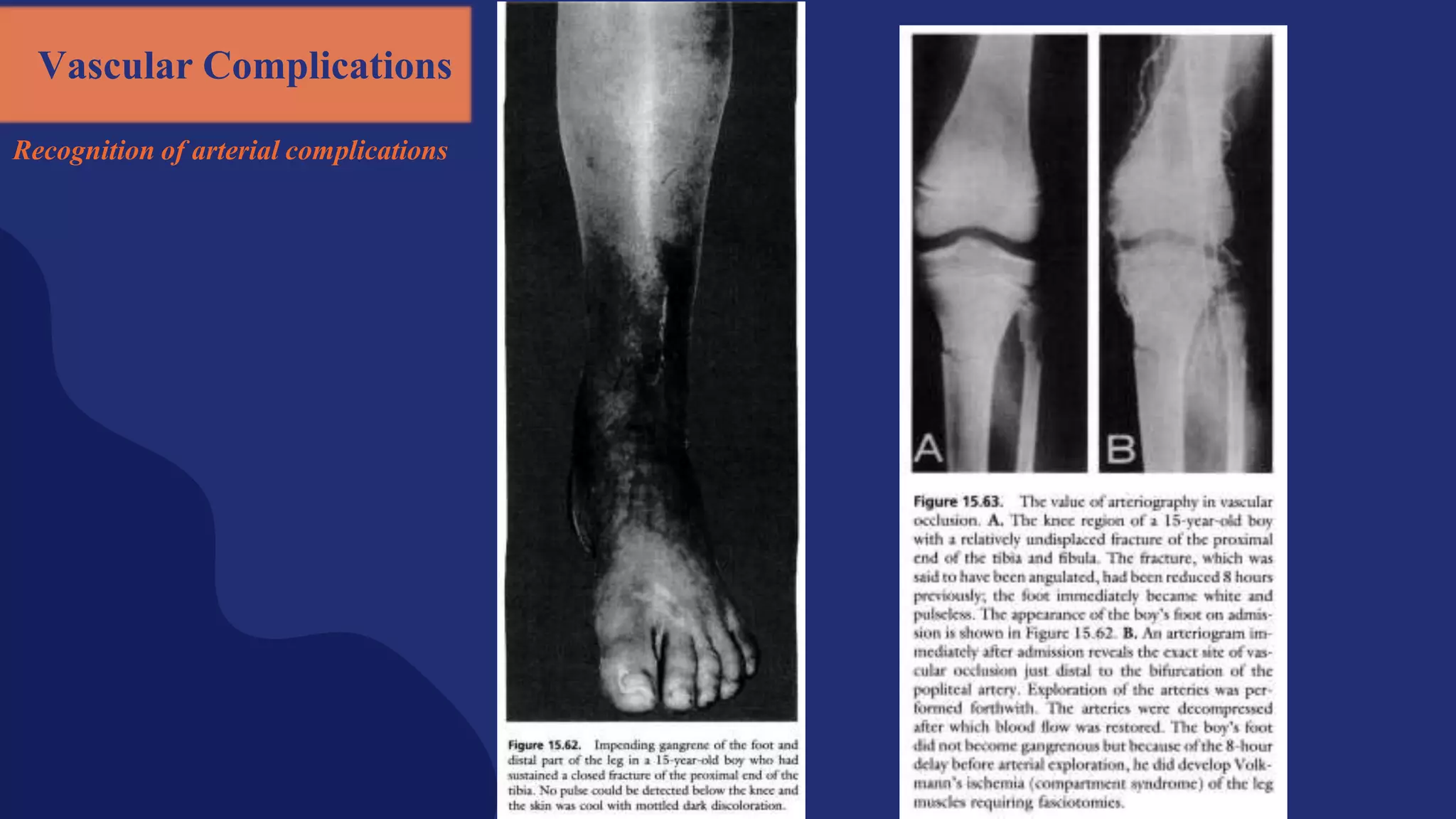
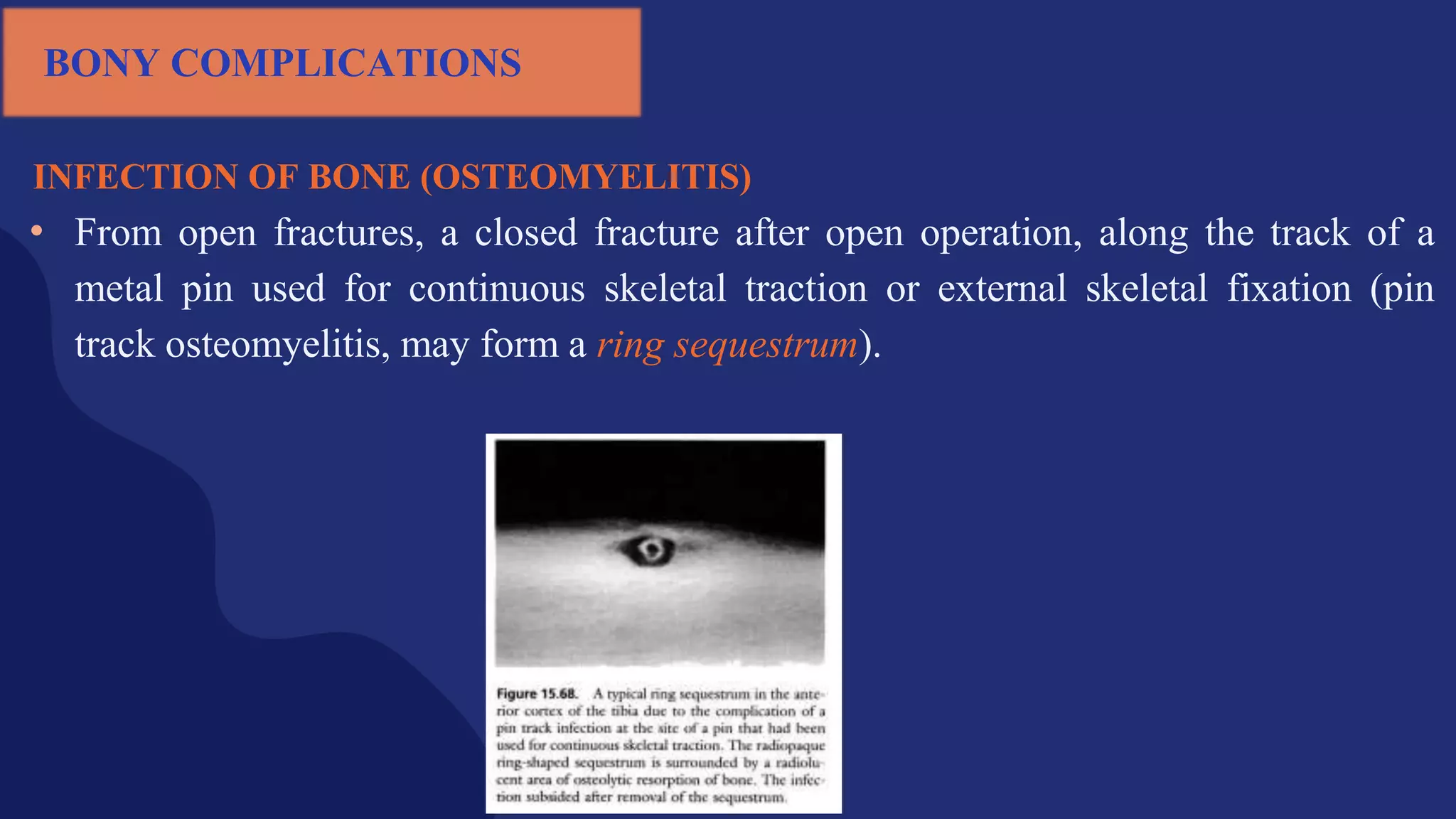
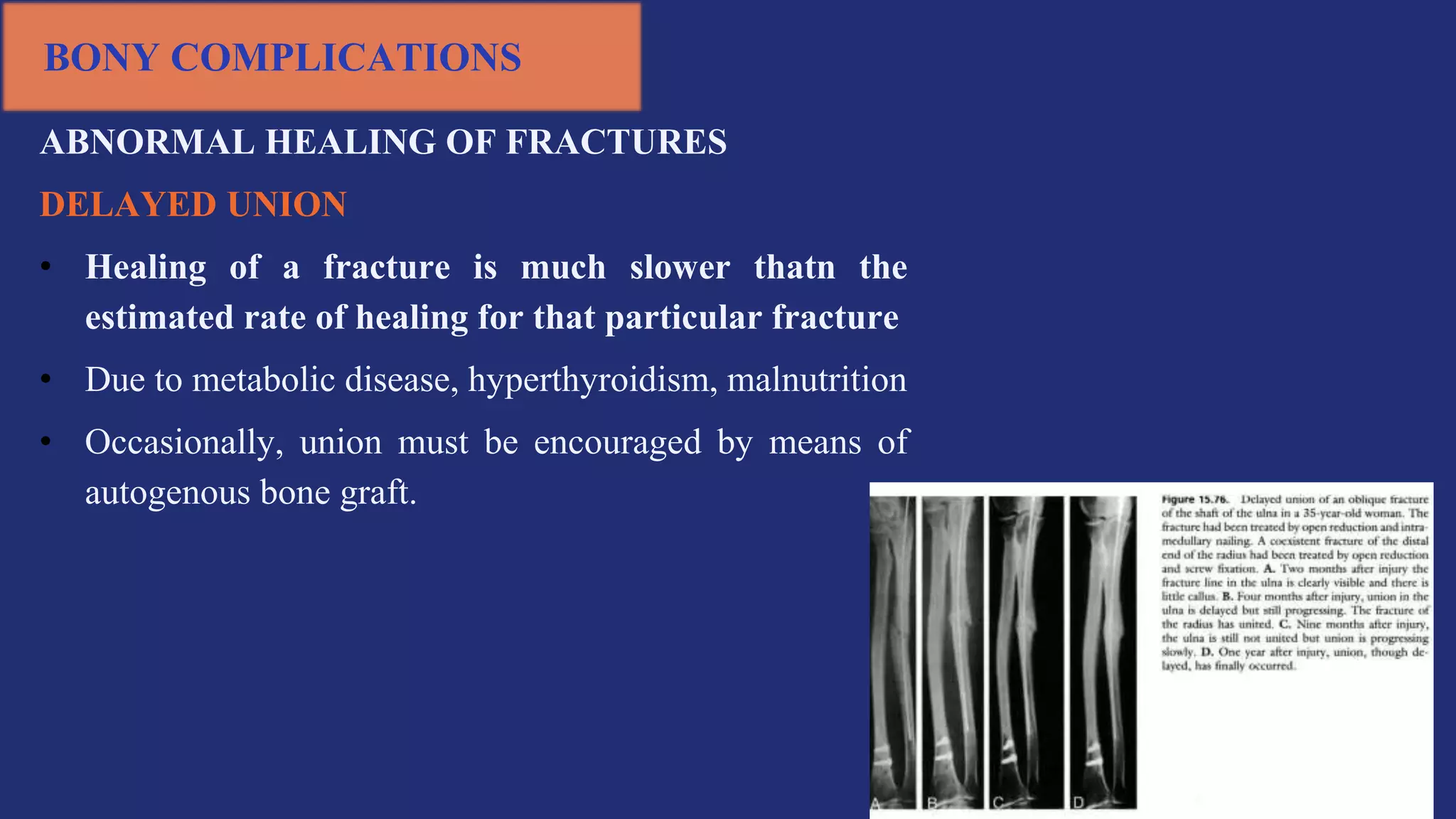
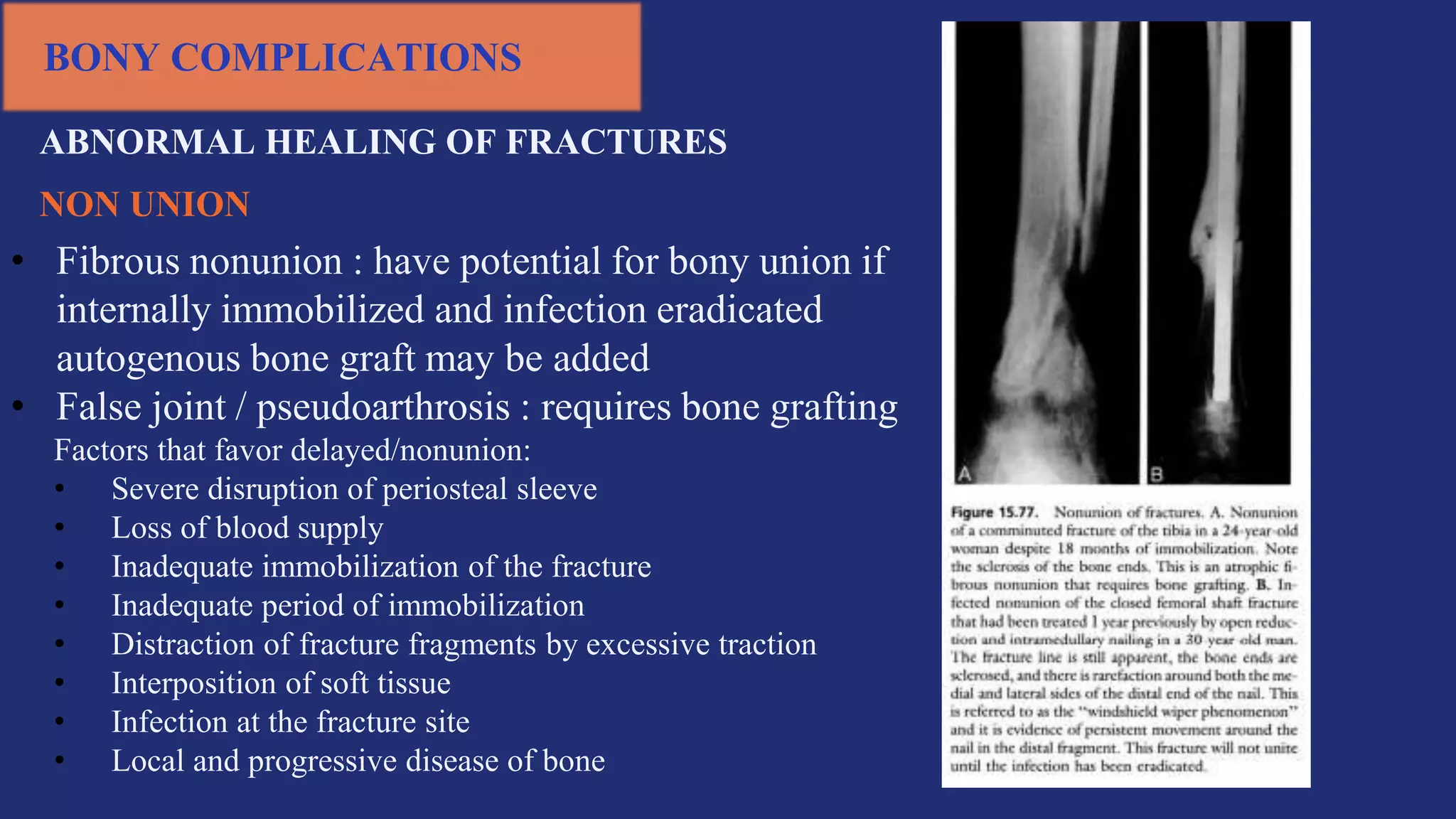
Fractures and joint injuries pose a significant health burden. The annual cost of trauma in North America is over $160 billion. Fractures occur due to physical forces that cause the bone to bend, twist, or pull apart. Associated soft tissue injuries can also occur, affecting organs like the brain, spinal cord, blood vessels, or nerves. Fracture healing involves inflammation, formation of a soft and then hard callus, and remodeling. Complications can include malunion, delayed or non-union, infection, or problems with joints. Careful diagnosis and treatment aim to restore normal function.