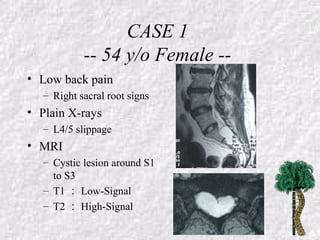
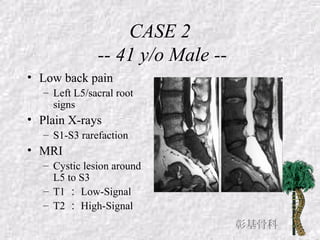
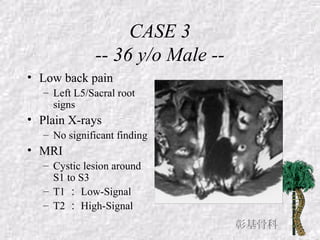
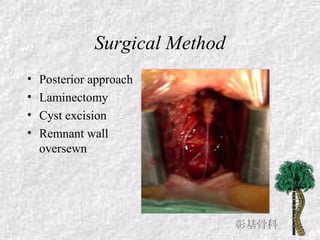
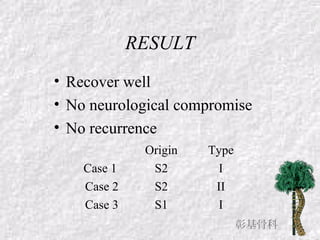
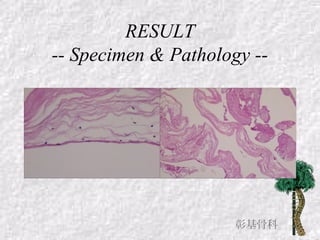
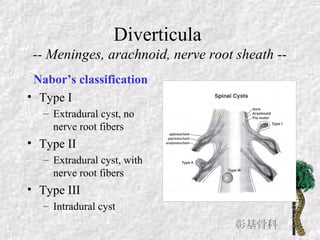
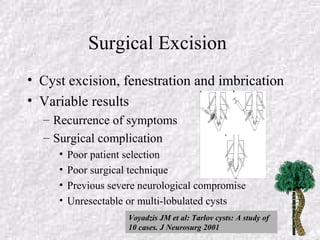
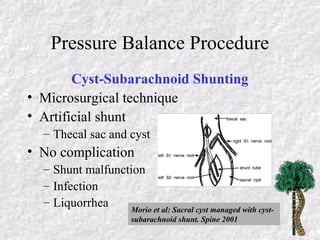
This document reports on 3 cases of symptomatic sacral cysts treated with surgical excision and discusses sacral cysts and their treatment options. Sacral cysts are uncommon lesions that can cause low back pain and neurological symptoms. Diagnosis involves imaging like CT myelography or MRI. Surgical intervention includes excision for well-encapsulated cysts to preserve nerve roots or pressure balance procedures for large or multi-lobulated cysts where complete excision is impossible and nerve roots may need sacrificing. Percutaneous procedures are no longer recommended due to high failure and complication rates.