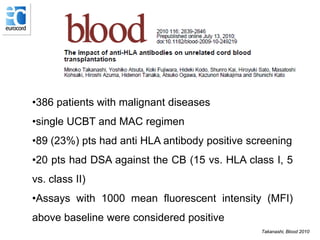
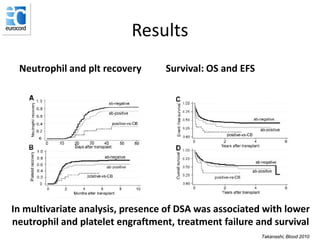
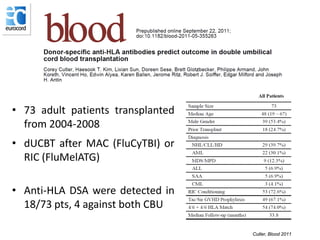
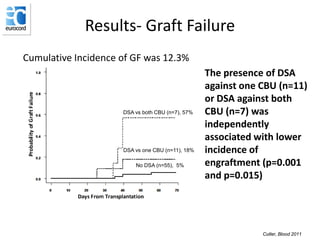
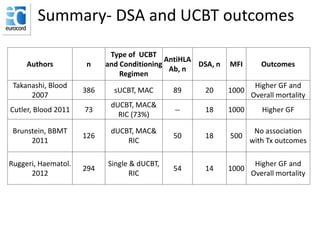
1) Several studies have found that the presence of donor-specific anti-HLA antibodies (DSA) in cord blood transplant recipients is associated with worse transplant outcomes, including higher rates of graft failure and mortality.
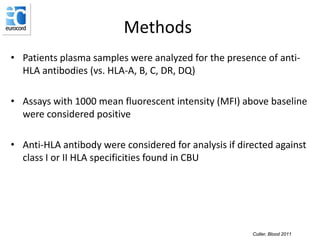
2) The intensity of DSA as measured by mean fluorescent intensity (MFI) correlates with transplant outcomes, with higher MFI DSA generally leading to poorer engraftment and survival.
3) Screening recipients for DSA and avoiding the selection of cord blood units with antigens corresponding to identified DSA is recommended to improve outcomes after cord blood transplantation.