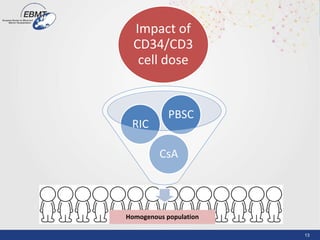
1) The document summarizes findings from multiple studies comparing the use of bone marrow versus peripheral blood stem cells as the stem cell source for haploidentical hematopoietic stem cell transplantation.
2) Results showed no significant differences in rates of acute or chronic graft-versus-host disease, non-relapse mortality, overall survival, or progression-free survival between the two stem cell sources.
3) Peripheral blood stem cells were associated with similar hematologic recovery times but were easier to collect and transplant compared to bone marrow.
















![18
CD3 : multivariate model
Variables adjusted by Age, donor, HCT-CI, DRI, CD34
HR 95CI p
PFS 0.8 [0.56-1.17] 0.272
OS 0.8 [0.54-1.24] 0.346
NRM 0.8 [0.46-1.47] 0.512
0.8CIR [0.50-1.30] 0.352
AGVHD III-IV 0.8 [0.36-1.68] 0.526
CGVHD Extensive 1.1 [0.65-1.93] 0.668
CD3
≥ median](https://image.slidesharecdn.com/1140-1200didierblaiseupdate1508-28-pbsc-bangkok-150828101041-lva1-app6892/85/Peripheral-Blood-Stem-Cell-Transplant-18-320.jpg)










