The document discusses cardiac rhythms and monitoring. It provides information on:
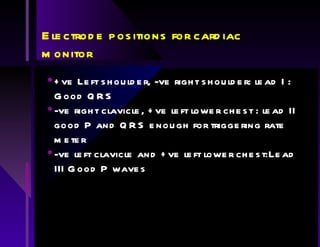
1) Electrode placements for cardiac monitoring and which leads are best for viewing different waveforms like P waves and QRS complexes.
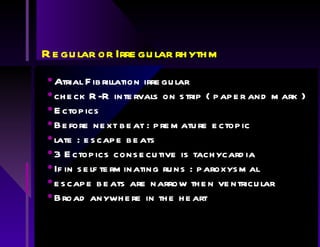
2) How to interpret a rhythm strip by examining features like heart rate, rhythm regularity, presence of atrial activity, and relationship between atrial and ventricular rhythms.
3) Causes and characteristics of different cardiac rhythms like bradycardias, tachycardias, conduction abnormalities, and rhythms associated with cardiac arrest.