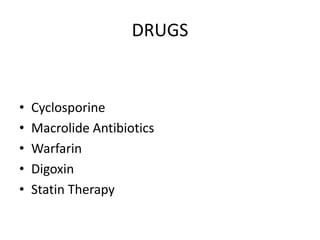
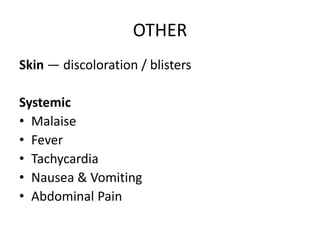
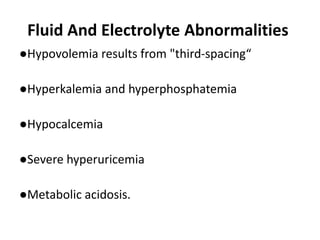
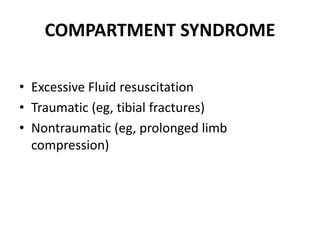
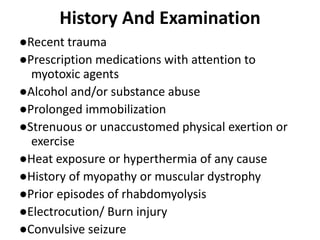
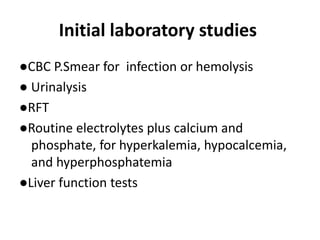
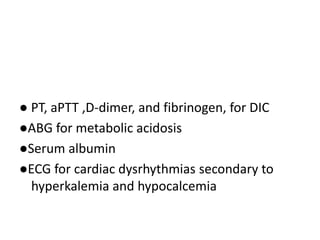
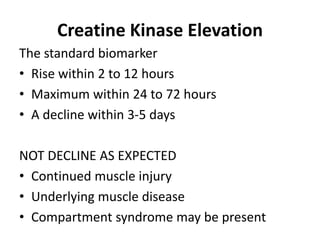
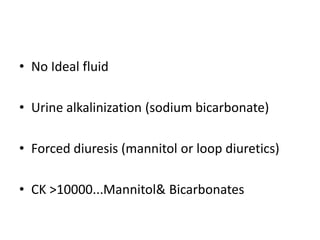
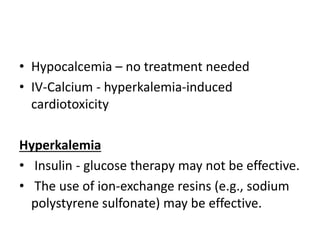
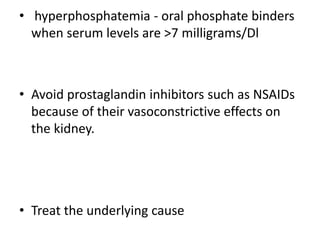
Rhabdomyolysis is a syndrome characterized by muscle necrosis and the release of intracellular muscle constituents into circulation. Common causes include drugs, medications, muscle diseases, trauma, infections, strenuous activity, and heat illness. Clinical manifestations range from asymptomatic enzyme elevations to life-threatening illness. Diagnosis is based on elevated creatine kinase levels and management focuses on aggressive IV fluid resuscitation to prevent acute kidney injury from electrolyte abnormalities that can result.