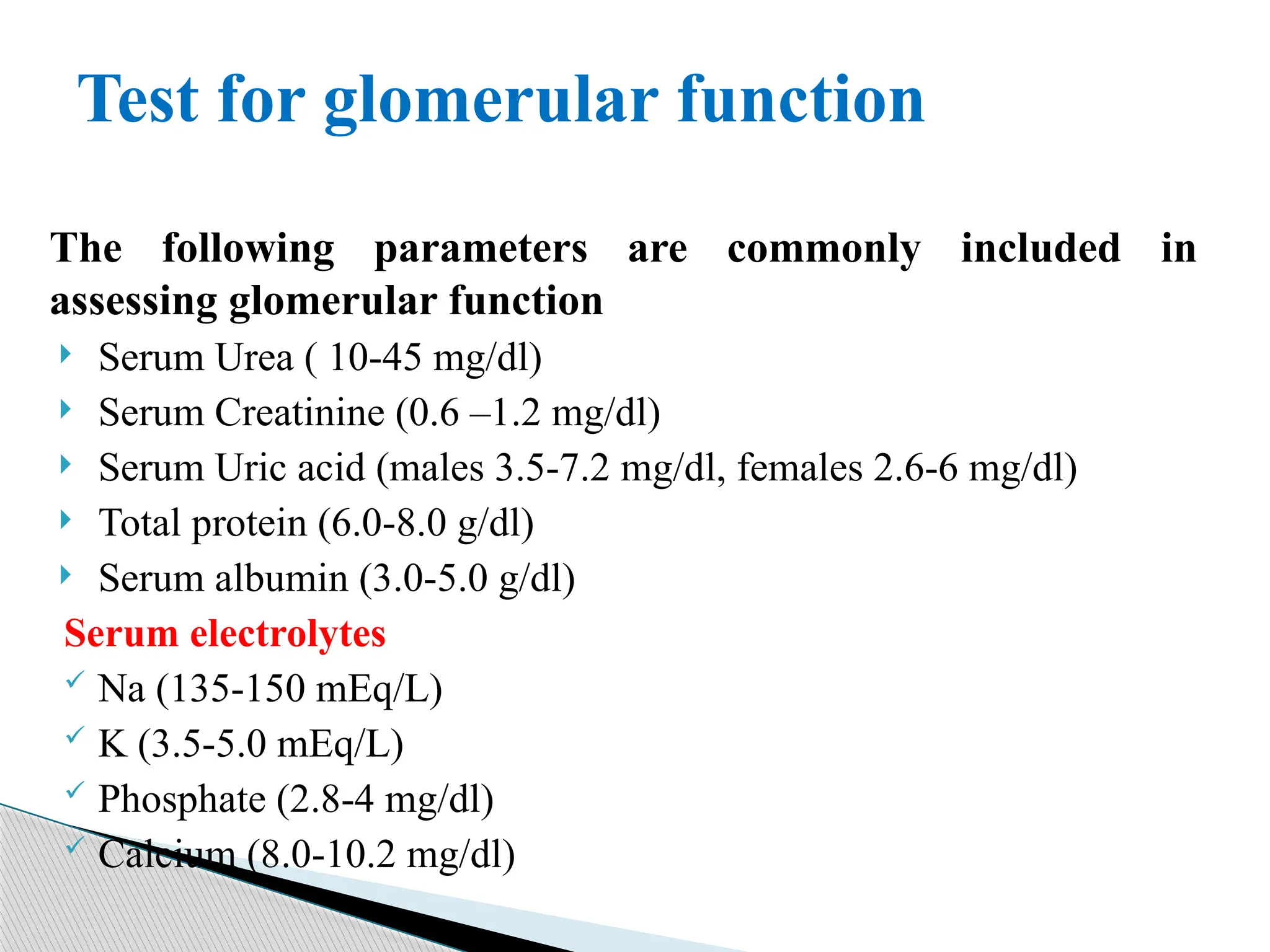
The renal function test (RFT) is a group of assessments used to evaluate kidney functionality, diagnose renal impairment, and monitor treatment effectiveness. It includes tests for glomerular and tubular function, focusing on parameters such as serum urea, creatinine, and electrolytes, with specific reference ranges provided. Abnormal values of these parameters can indicate various conditions, including dehydration, renal failure, and electrolyte imbalances.