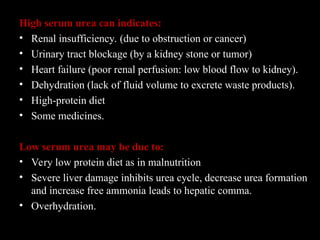
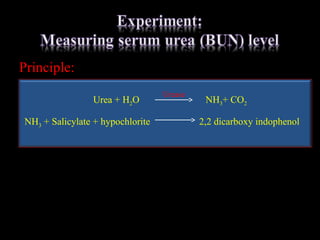
The document details the functions of the renal system, emphasizing its roles in excretion, homeostasis, and hormone production, specifically outlining the structure and functioning of nephrons. It explains urine formation through glomerular filtration, tubular reabsorption, and secretion, along with various kidney function tests and factors affecting kidney health. Additionally, it addresses the interpretation of biochemical tests related to kidney function, including the implications of abnormal results and the relationship between urea levels and renal dysfunction.