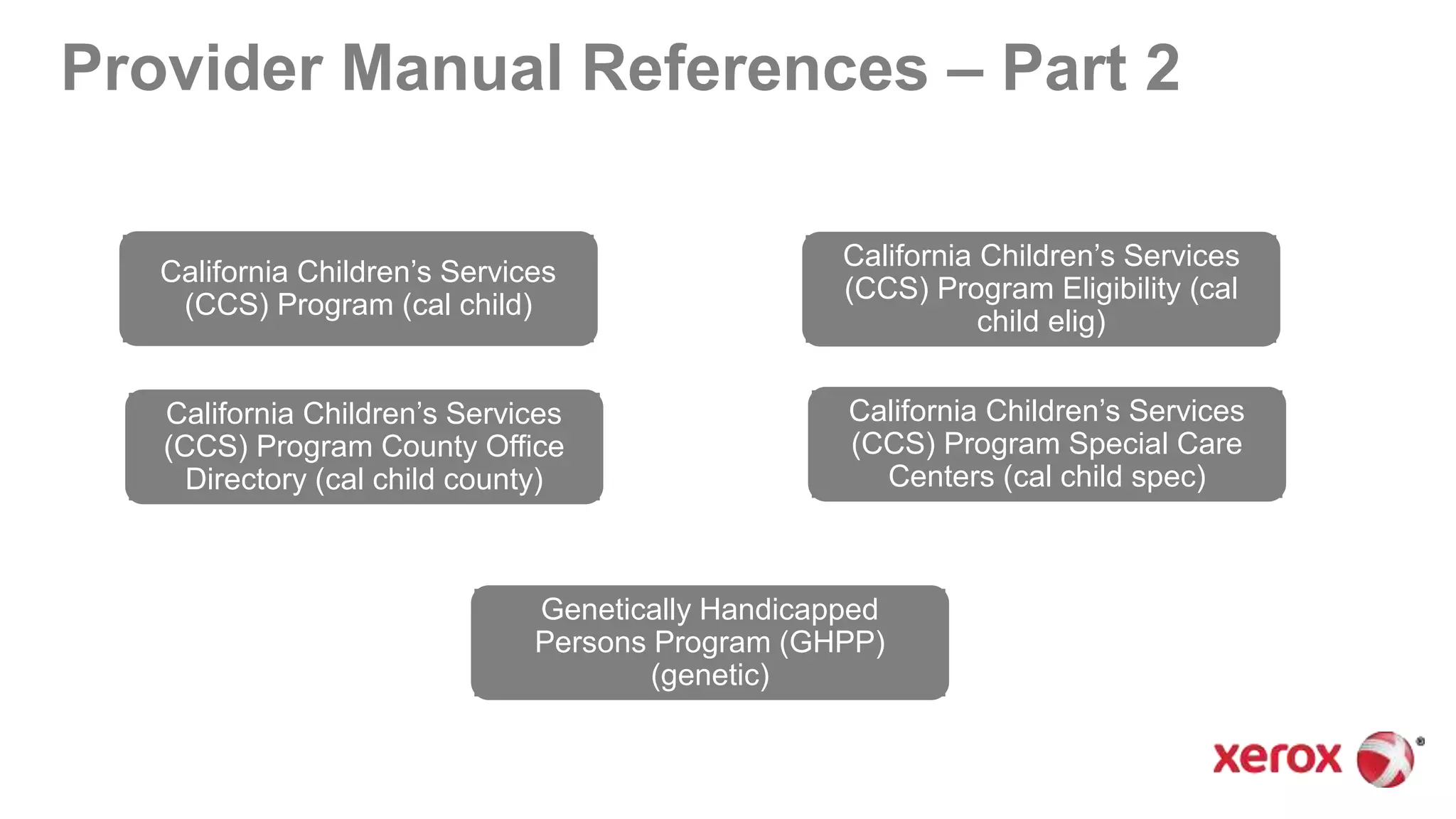
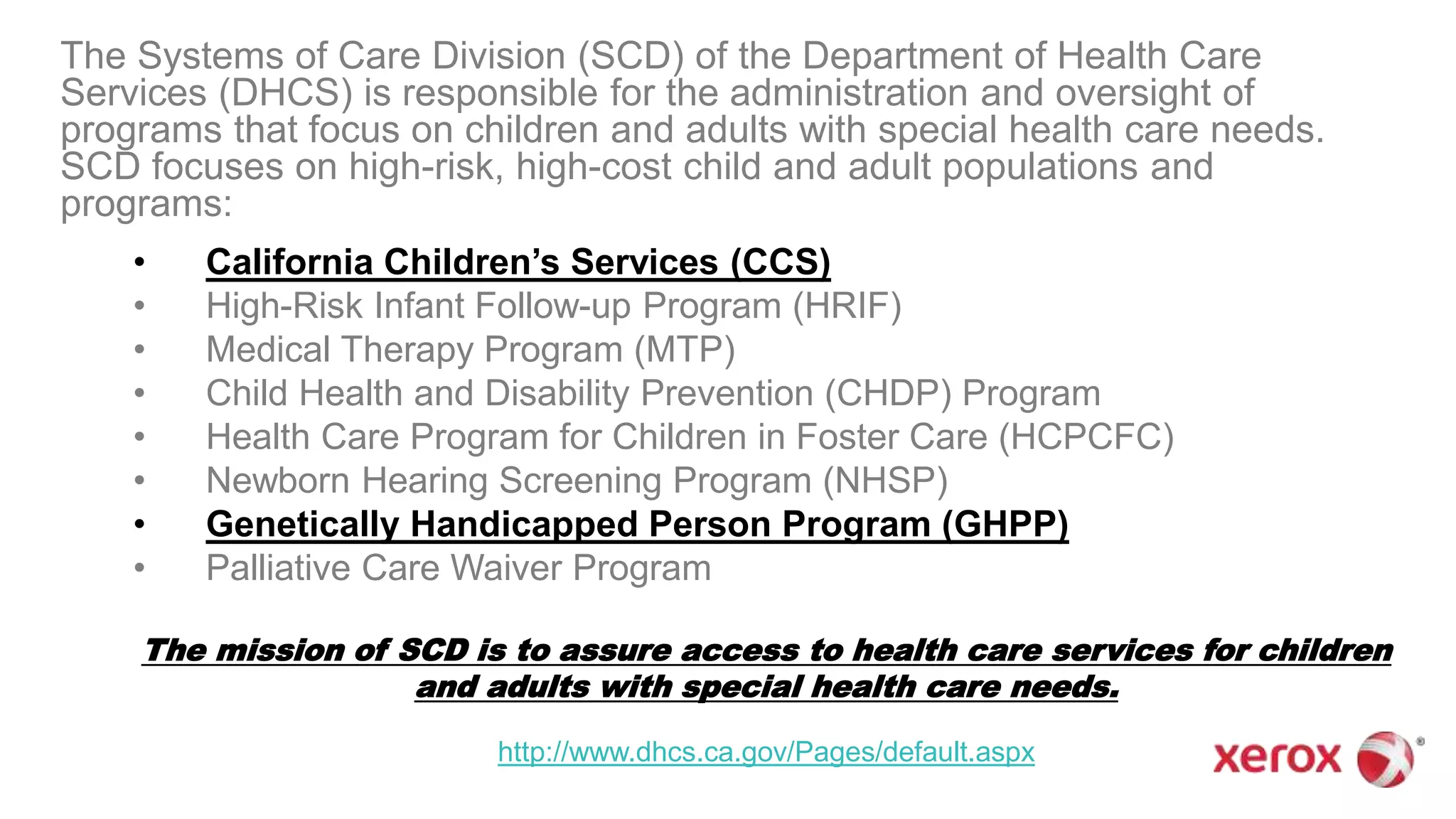
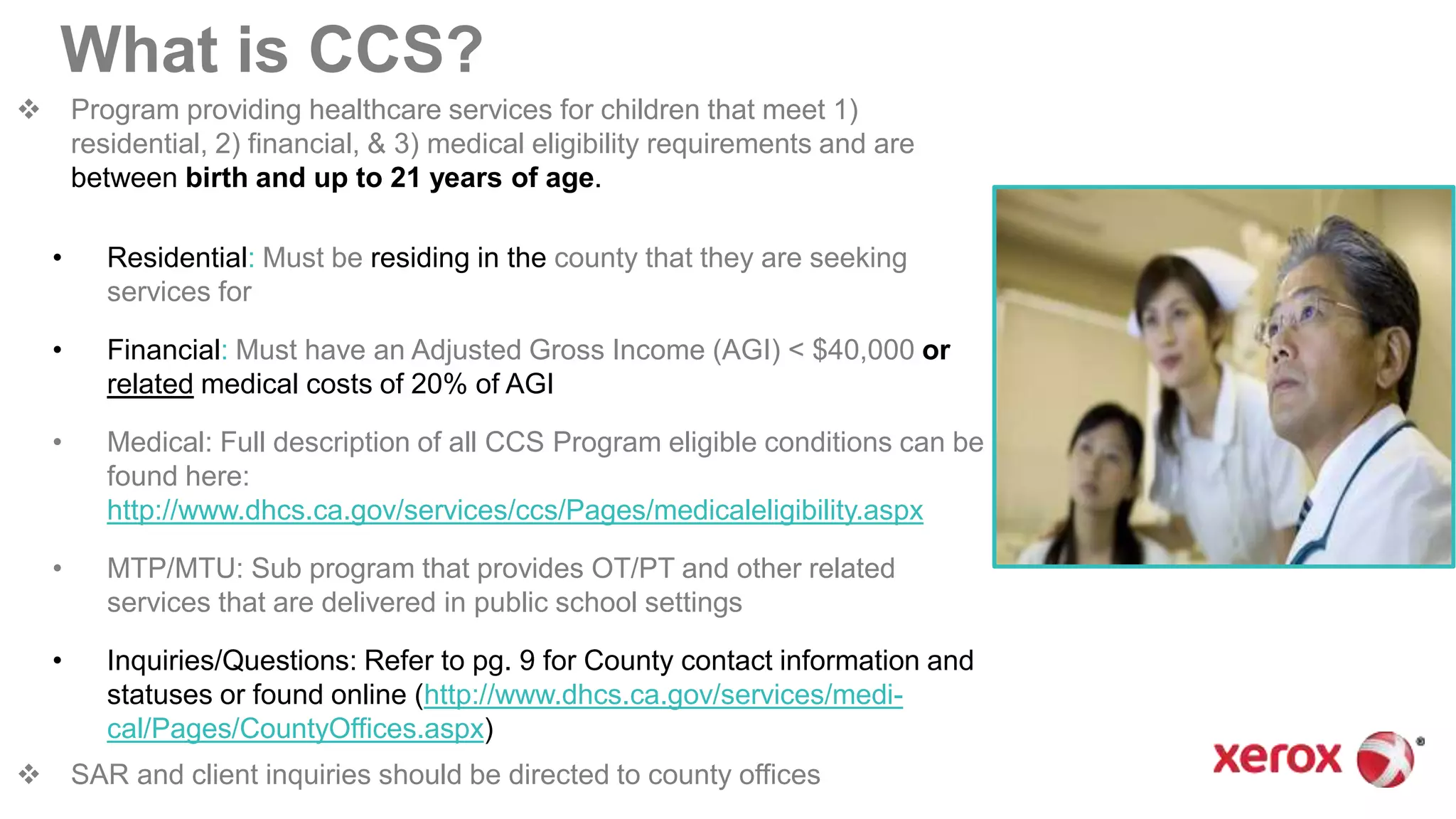
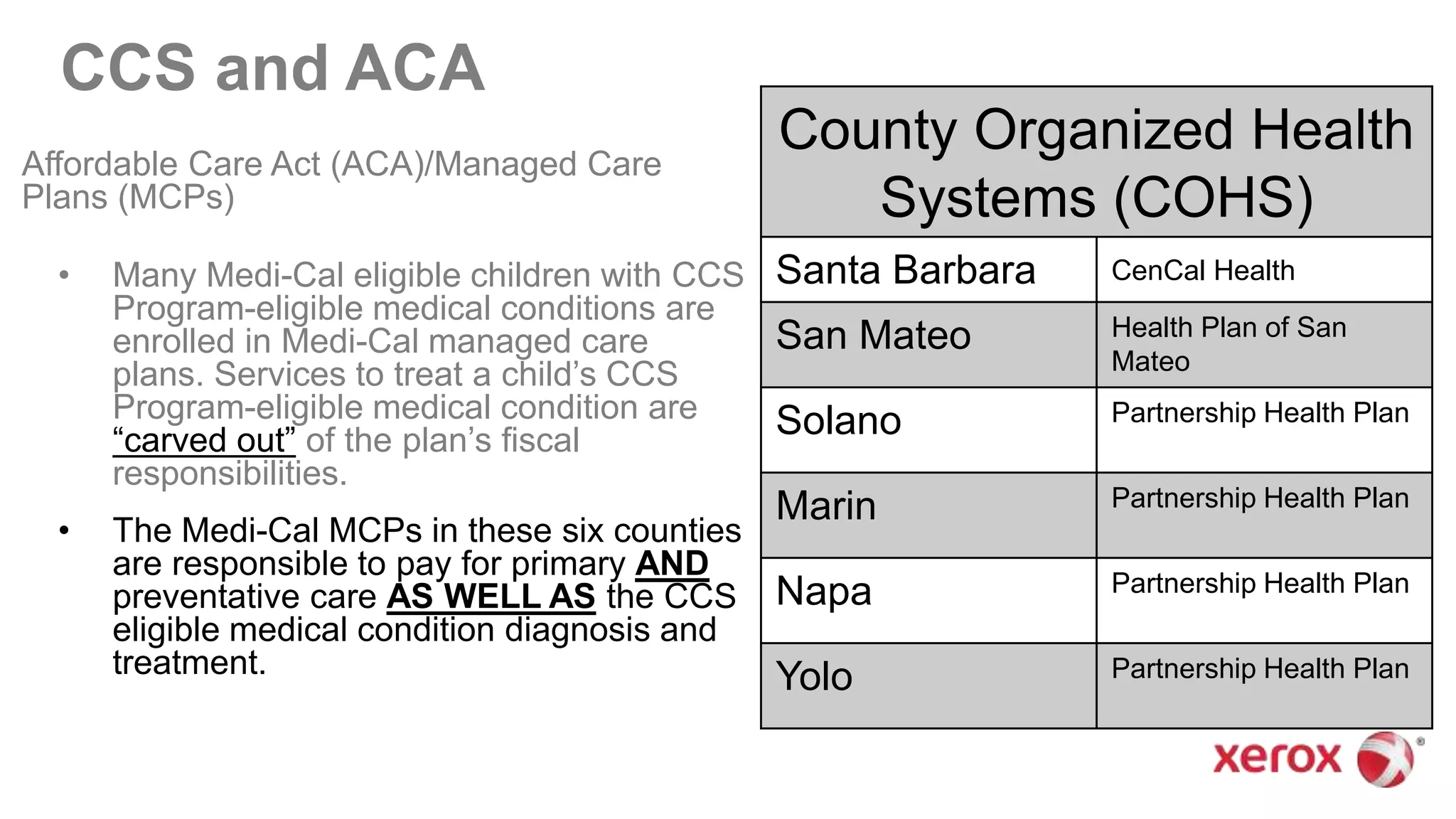
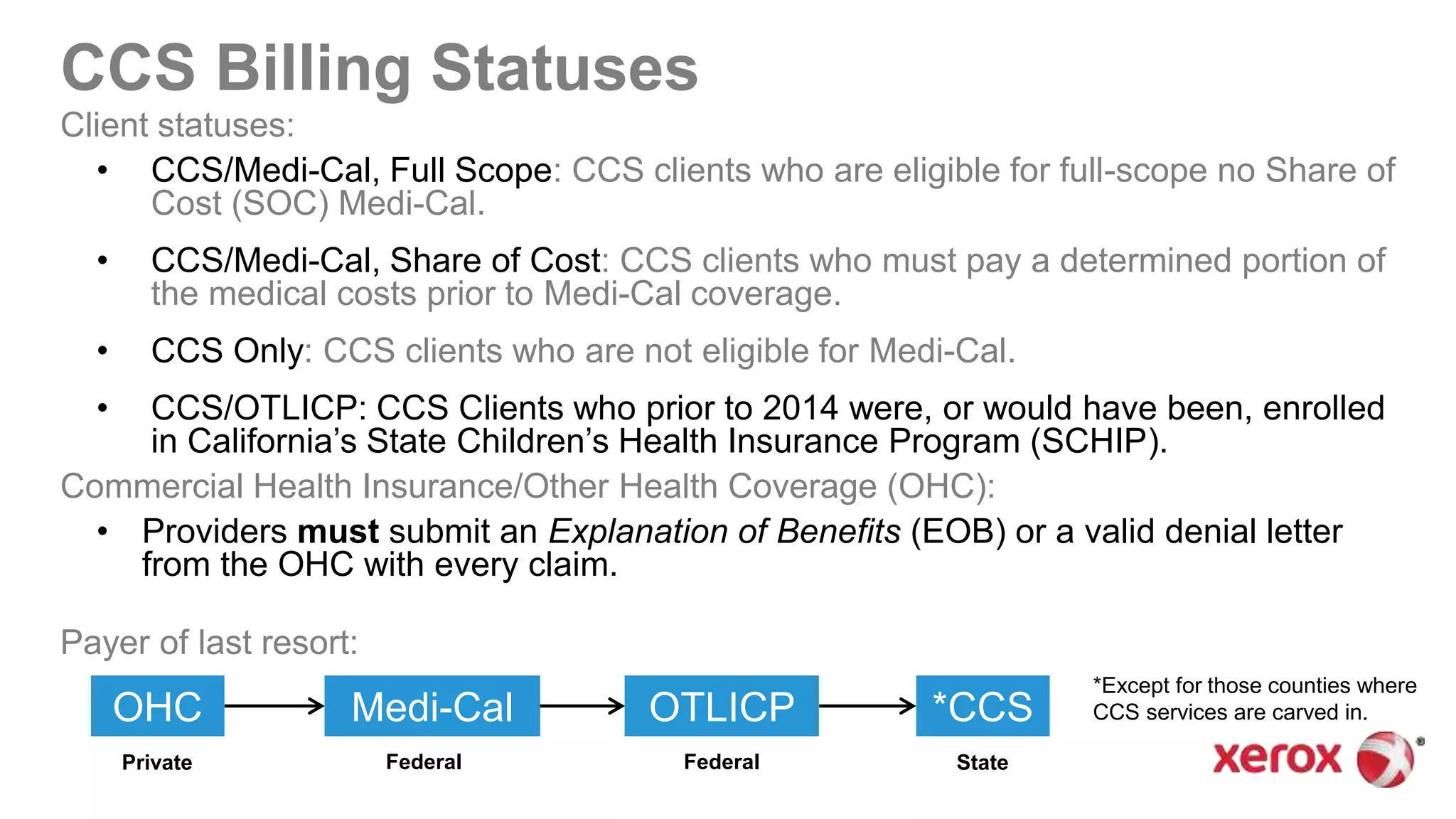
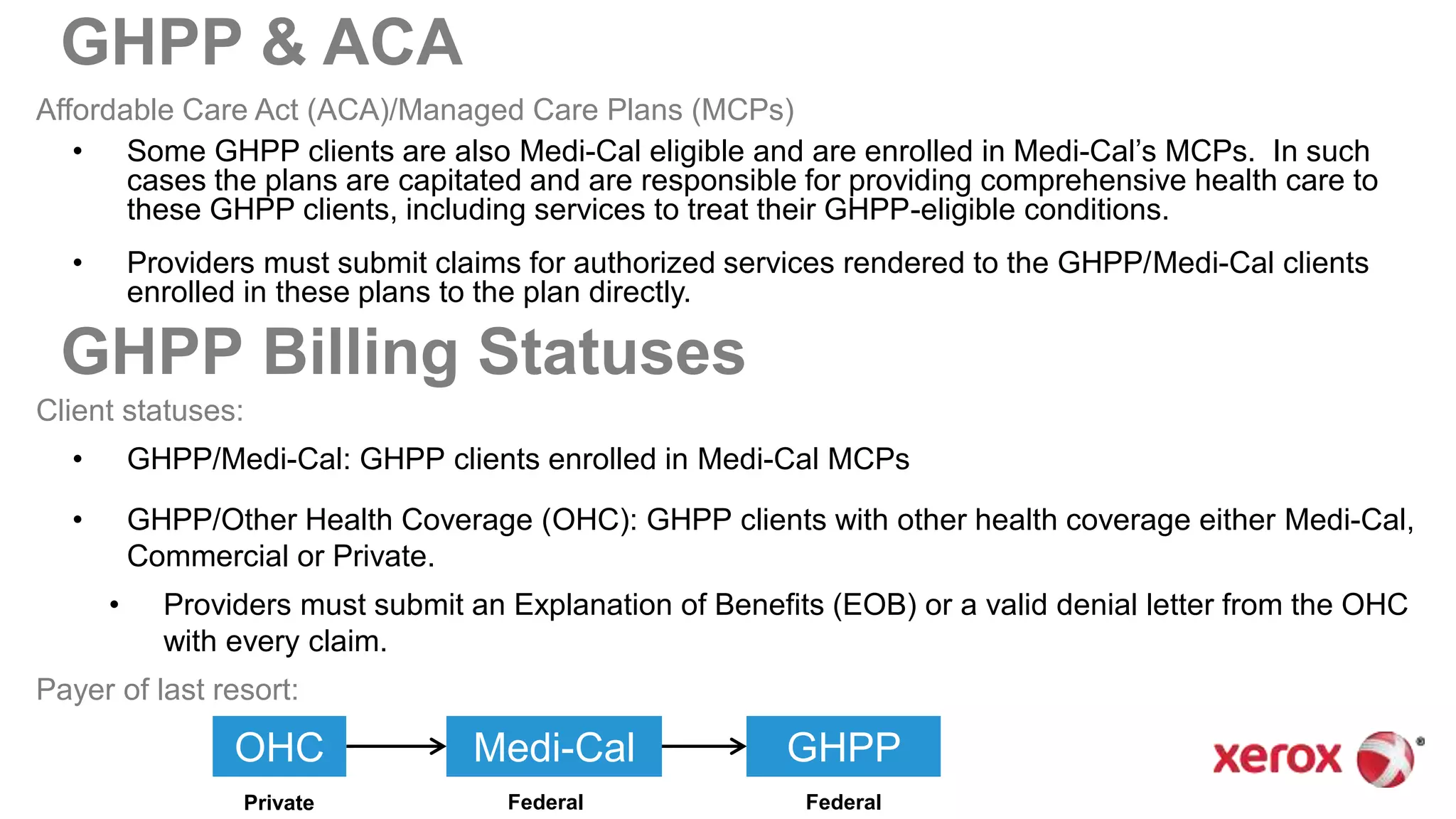
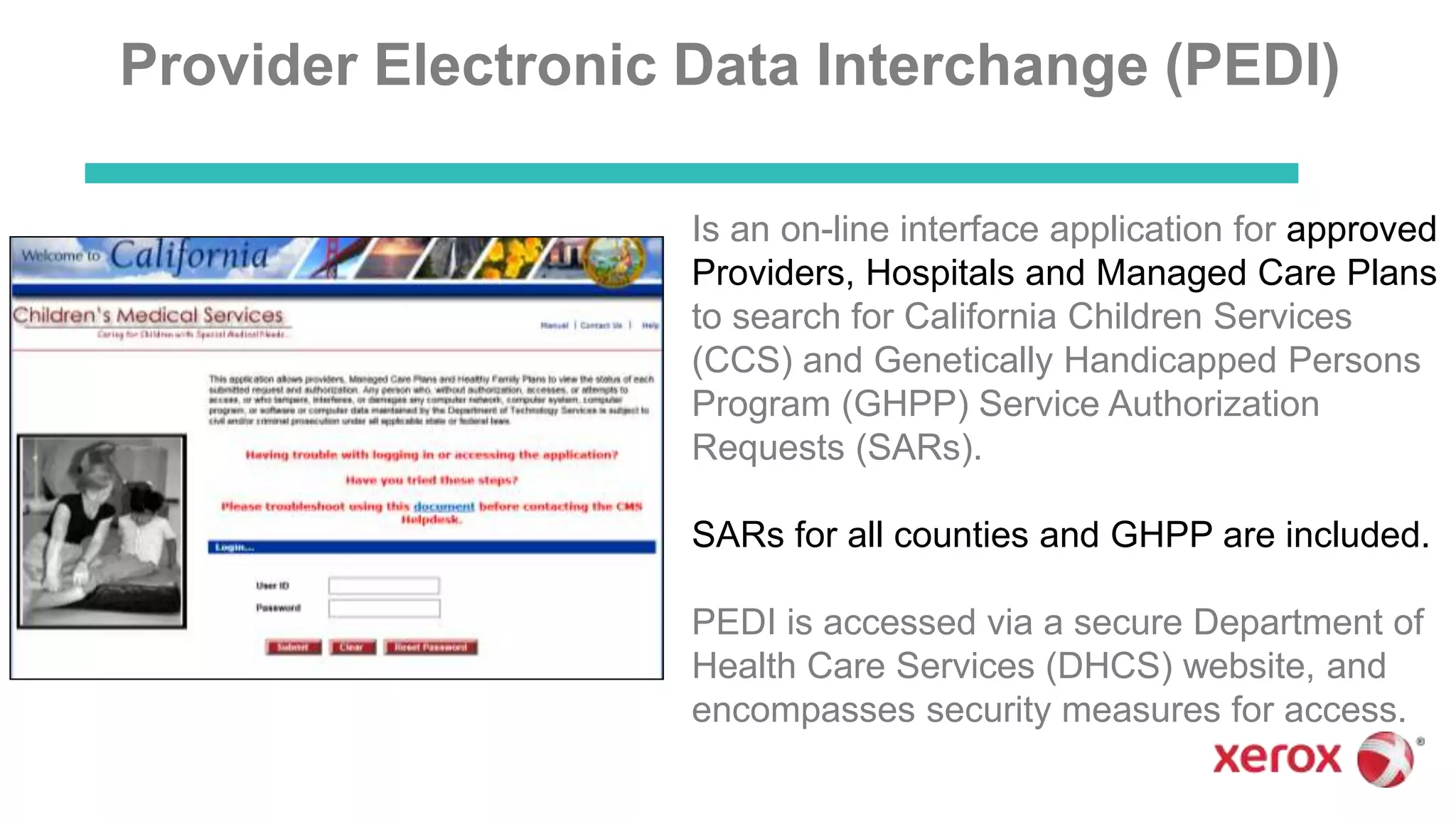
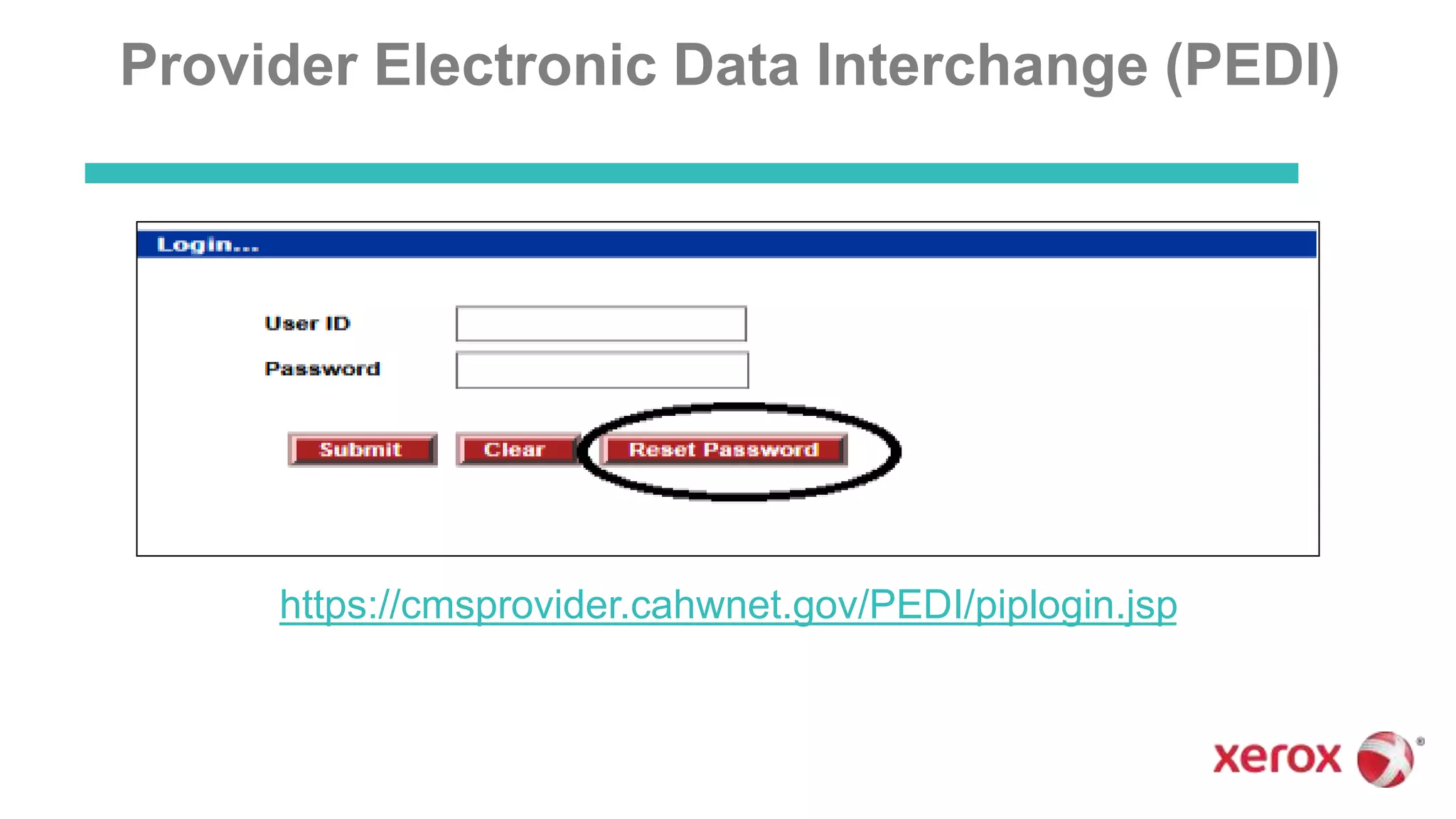
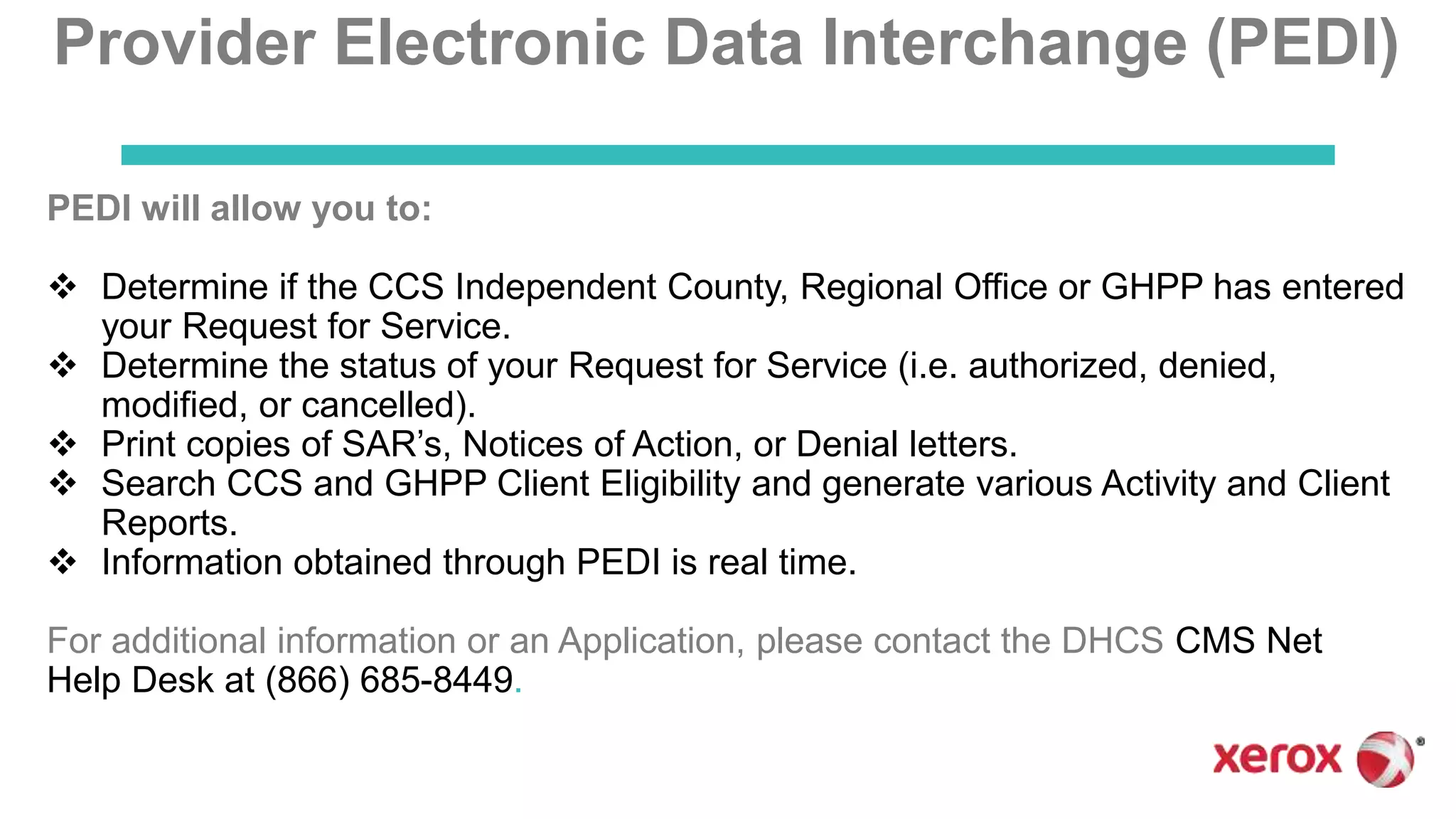
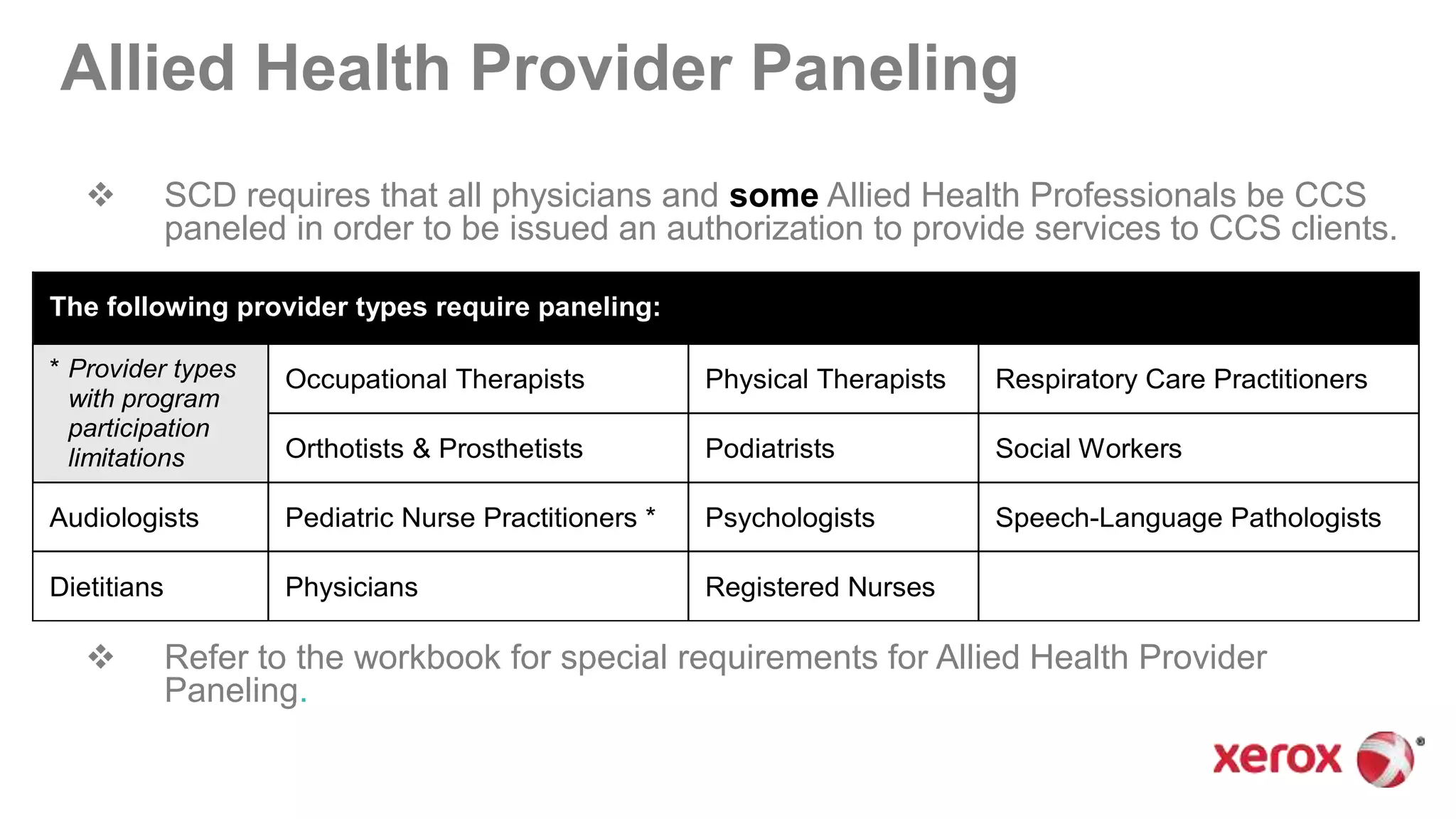
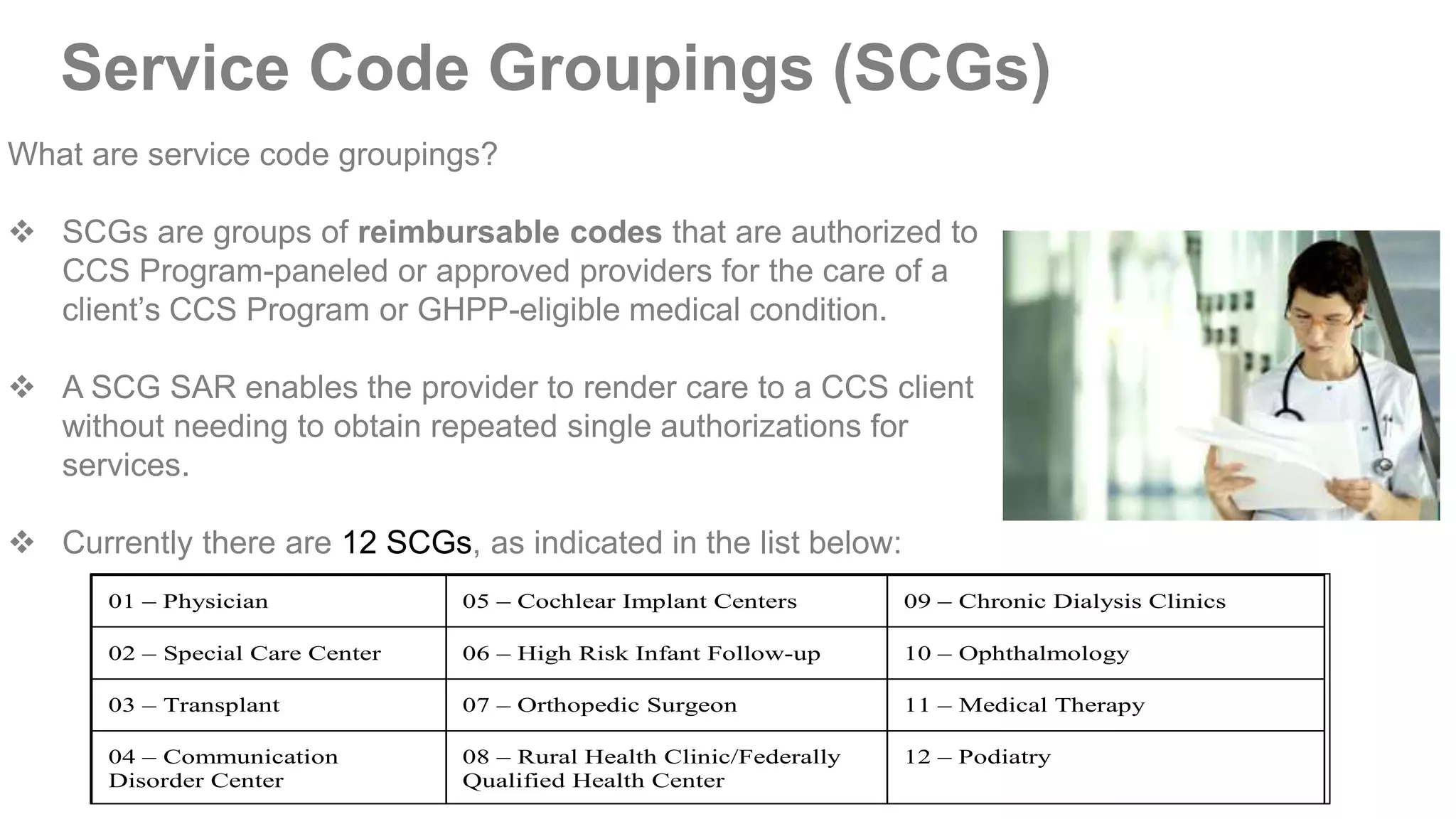
This document provides an overview of the California Children's Services (CCS) Program and the Genetically Handicapped Persons Program (GHPP). It discusses eligibility requirements, covered services, referral processes, billing statuses, and the roles of providers. Key points include that CCS serves children with certain medical conditions who meet residential, financial, and medical eligibility, while GHPP serves adults with specified genetic diseases. Referrals are made to local CCS county offices or the state GHPP office by submitting a Service Authorization Request form. Providers must be paneled and authorized to provide services to CCS and GHPP clients.