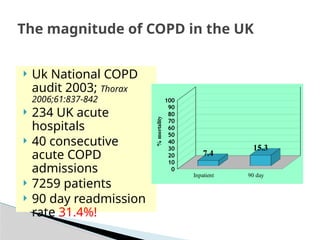
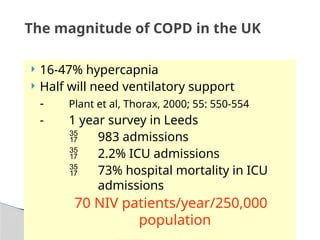
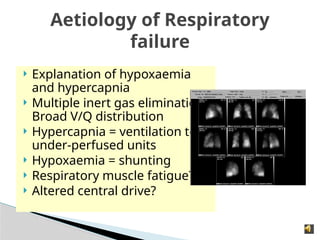
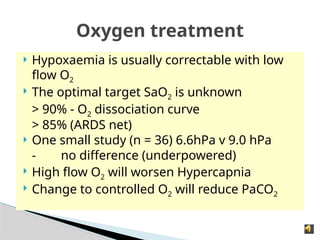
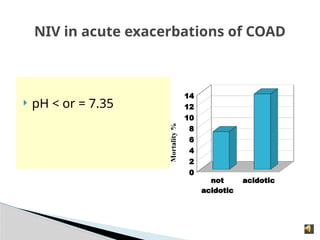
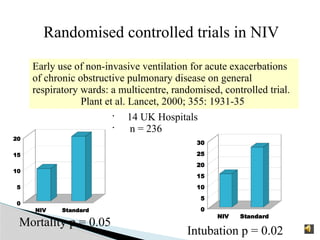
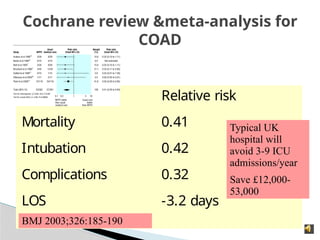
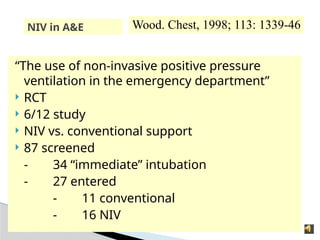
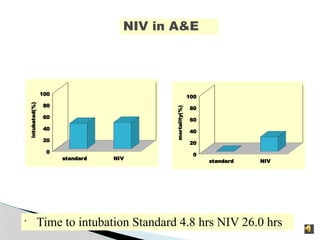
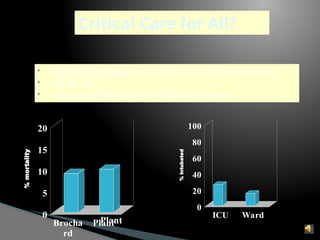
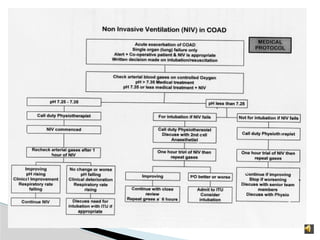
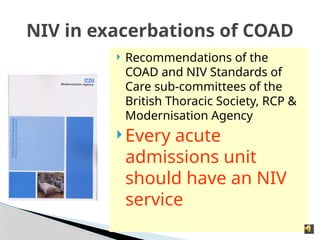
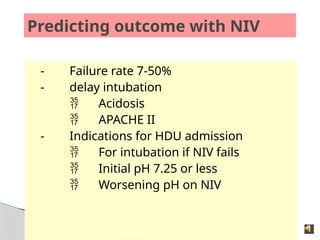
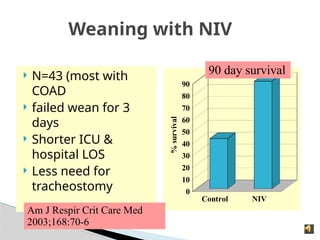
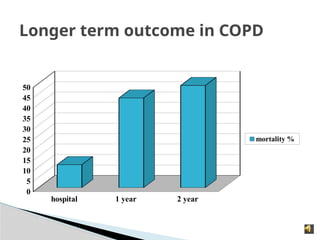
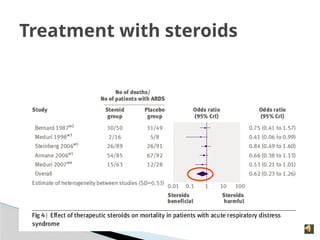
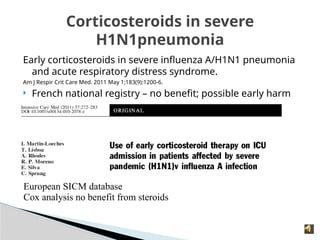
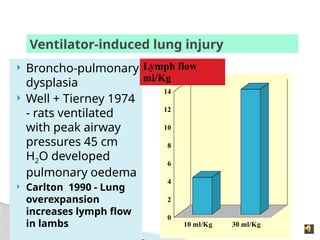
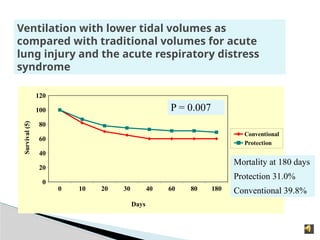
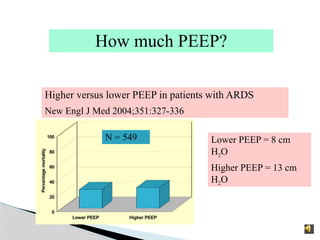
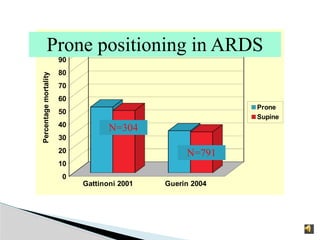
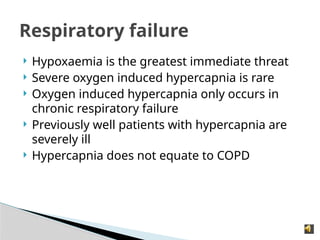
The document discusses management strategies for severe hypoxic respiratory failure, particularly in patients with chronic obstructive pulmonary disease (COPD) and highlights the efficacy of non-invasive ventilation (NIV) in improving survival and reducing intubation rates. It presents findings from various studies on the outcomes of COPD admissions, guidelines for oxygen treatment, and the use of corticosteroids in respiratory distress. Additionally, it addresses the importance of patient choice in treatment decisions and the complexities of ventilatory support in critical care settings.