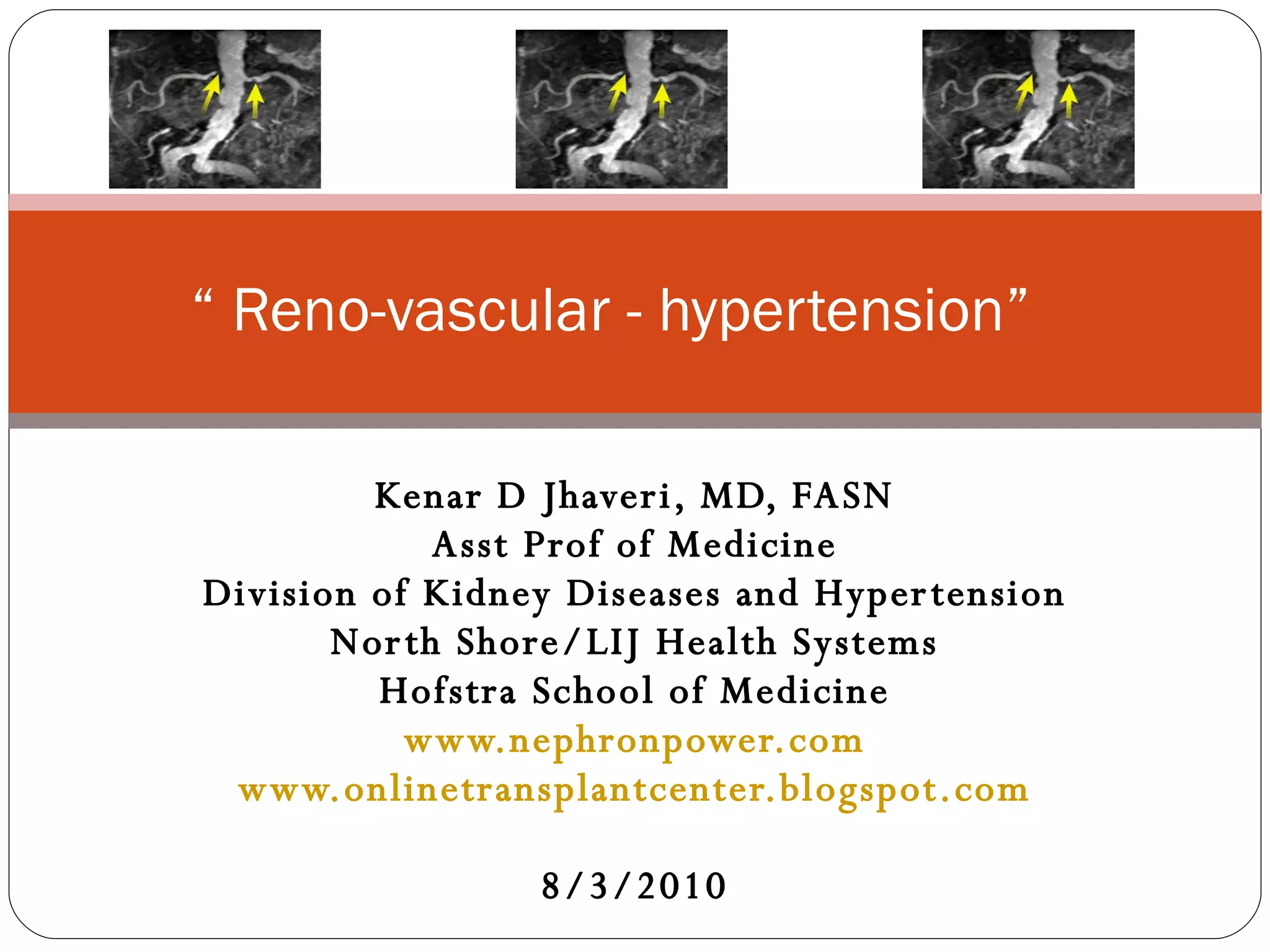
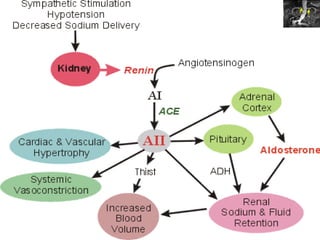
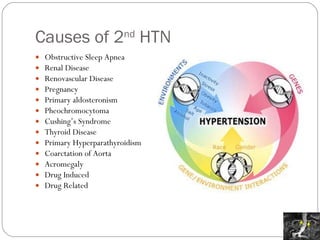
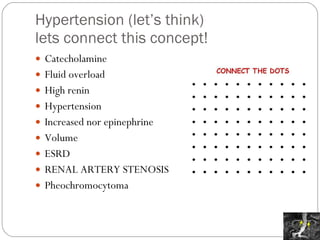
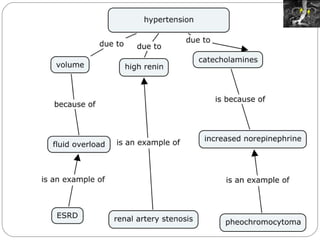
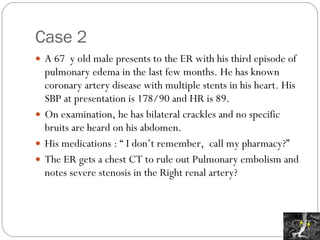
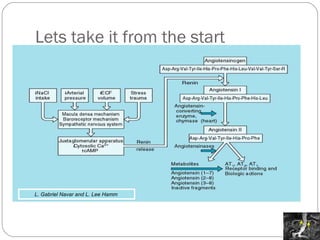
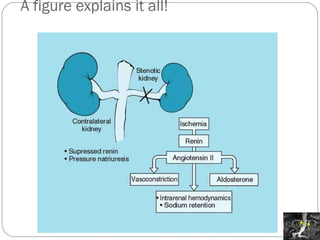
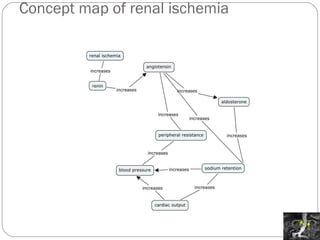
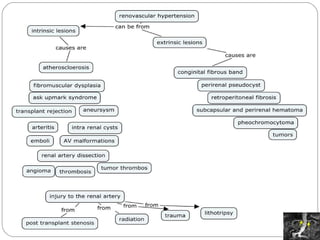
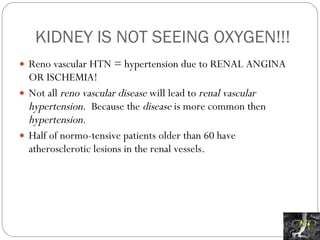
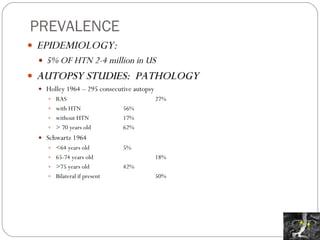
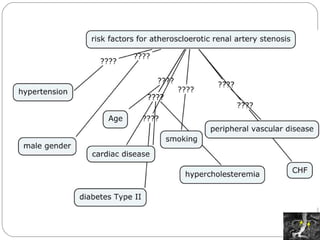
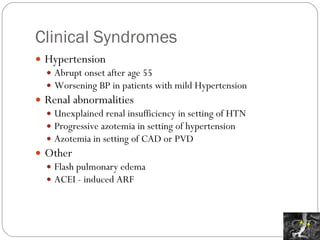
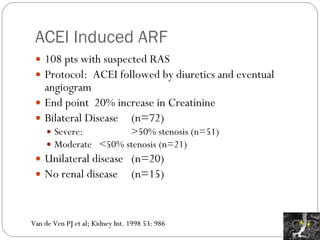
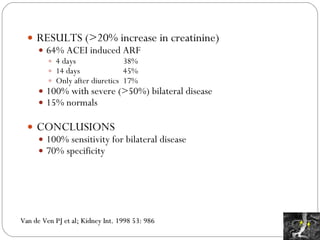
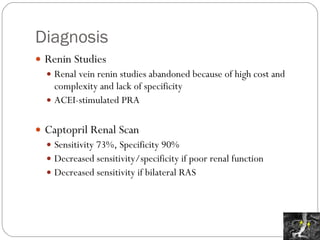
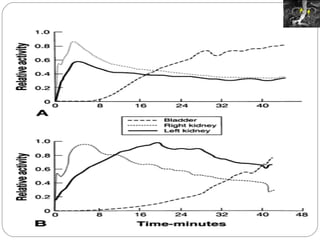
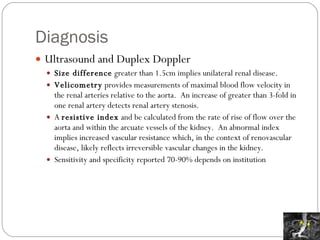
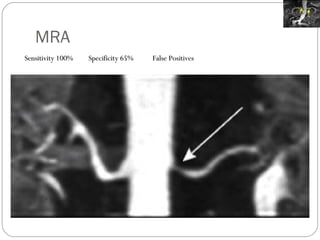
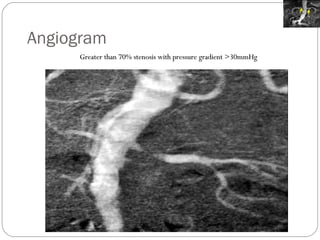
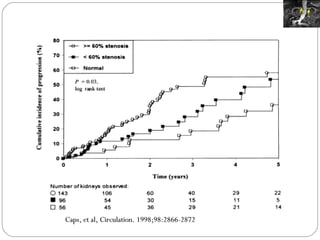
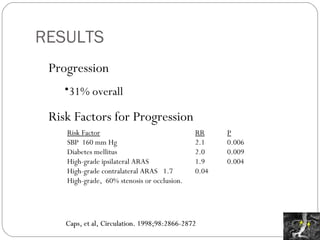
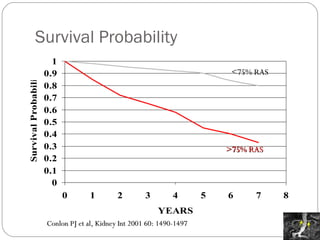
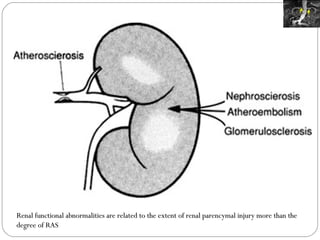
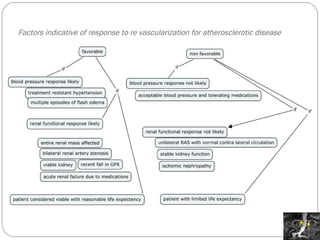
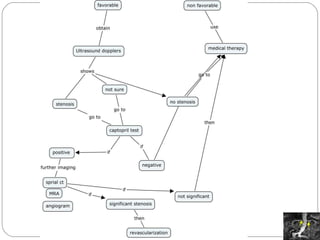
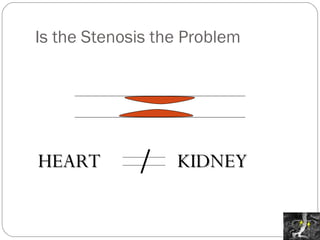
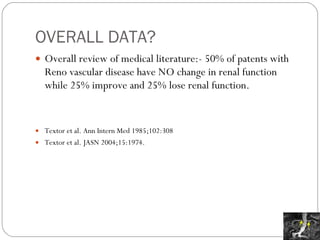
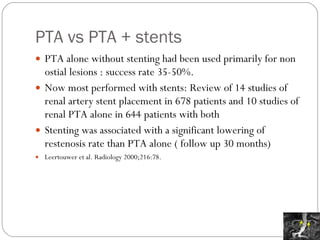
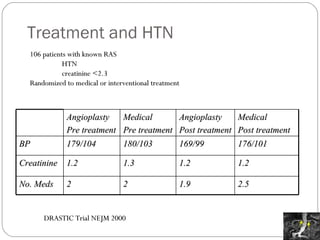
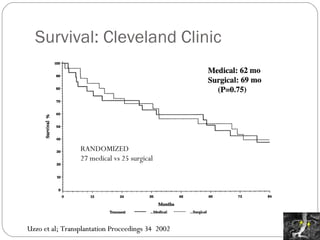
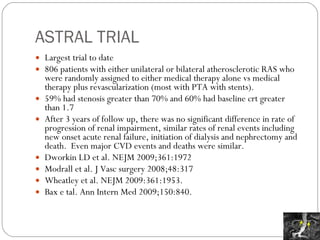
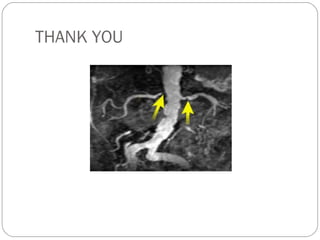
The document discusses renal vascular hypertension, highlighting the urologist's role in understanding its medical management due to its prevalence and implications during procedures such as donor nephrectomy. It includes case studies illustrating various causes of hypertension related to renal disease and outlines the progression and treatment options for atherosclerotic renal artery disease. The importance of recognizing hypertensive conditions and appropriate management strategies is emphasized for optimal patient outcomes.