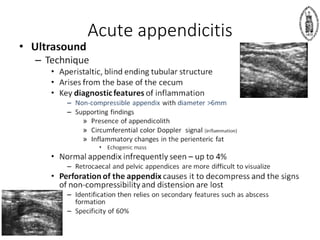
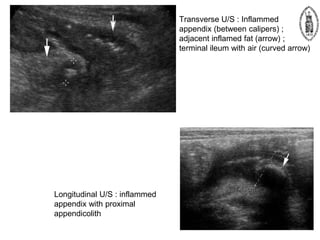
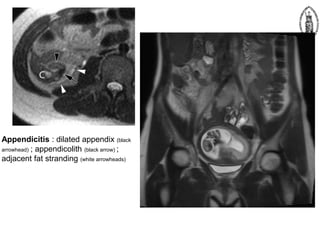
1) This case involves a 22-year-old man who presented with abdominal pain and was found to have early acute appendicitis on ultrasound.
2) Despite having minimal clinical symptoms and a normal blood test, ultrasound was repeated and again found evidence of early acute appendicitis.
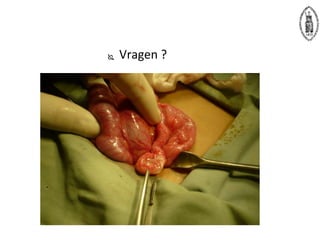
3) The patient was admitted for a laparoscopic appendectomy.