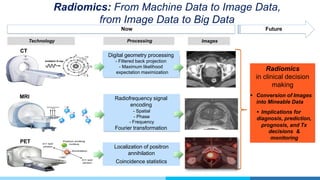
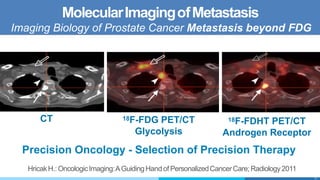
This document discusses the history and current state of imaging prostate cancer. It describes how imaging techniques have evolved from ultrasound and X-ray to current multiparametric MRI techniques. MRI is now used for detection, localization, staging, treatment planning and follow-up. The document outlines PI-RADS scoring and its role in standardizing prostate MRI reporting. It discusses indications for MRI and the added value of different MRI sequences. The document also examines radiomics and molecular imaging techniques for characterizing and detecting prostate cancer metastases. Overall, the document provides a comprehensive overview of the progress and ongoing work in imaging prostate cancer.






















![Prostate Cancer: Radiopharmaceuticals produced (and in translation) by the MSK
RMIP Core over the last 5 years. First-in-Human IND’s are highlighted in italics.
Radiopharmaceutical Imaging Target Cancer Site Human studies
Small Molecules (Imaging)
[18
F]-FLT tumor cell proliferation Lymphoma, prostate, H&N, NSCLC MSKCC IND 104742
[18
F]-FDHT androgen receptor Prostate MSKCC IND 66115
[18
F]-FACBC amino acid metabolism Breast, Prostate, Brain RDRC/ MSKCC IND 113970
[18
F]-FIAU gene expression Prostate MSKCC IND BB-IND 14028
[18
F]-FEAU gene expression All tumors and T-cell therapies MSKCC IND
[18
F]-dasatinib tyrosine kinases Prostate, Breast MSKCC IND 118697
[18
F]-glutamine tumor metabolism All solid malignancies MSKCC IND 116187
[124
I]-FIAU gene expression Prostate MSKCC IND BB-IND 14028
[124
I]-PUH71 HSP-90 All solid malignancies and lymphoma MSKCC IND 110291
[18
F]-FCholine Tumor cell proliferation Brain MSKCC RDRC
[11
C]-Choline Tumor cell proliferation Prostate MSKCC IND 127257
Antibodies and Fragments (Imaging)
[89
Zr]-DFO-huJ591 PSMA Prostate MSKCC IND 114077
[89
Zr]-DFO-MSTP2109A PSMA Prostate MSKCC IND 116724
Small Molecules (Imaging)
[18
F]-FLT tumor cell proliferation Lymphoma, prostate, H&N, NSCLC MSKCC IND 104742
[18
F]-FDHT androgen receptor Prostate MSKCC IND 66115
[18
F]-FACBC amino acid metabolism Breast, Prostate, Brain RDRC/ MSKCC IND 113970
[18
F]-FIAU gene expression Prostate MSKCC IND BB-IND 14028
[18
F]-FEAU gene expression All tumors and T-cell therapies MSKCC IND
[18
F]-dasatinib tyrosine kinases Prostate, Breast MSKCC IND 118697
[18
F]-glutamine tumor metabolism All solid malignancies MSKCC IND 116187
[124
I]-FIAU gene expression Prostate MSKCC IND BB-IND 14028
[124
I]-PUH71 HSP-90 All solid malignancies and lymphoma MSKCC IND 110291
[18
F]-FCholine Tumor cell proliferation Brain MSKCC RDRC
[11
C]-Choline Tumor cell proliferation Prostate MSKCC IND 127257
Antibodies and Fragments (Imaging)
[89
Zr]-DFO-huJ591 PSMA Prostate MSKCC IND 114077
[89
Zr]-DFO-MSTP2109A PSMA Prostate MSKCC IND 116724](https://image.slidesharecdn.com/hedvighricakimagingprostatecancer-181121151025/85/Radiomics-in-Oncology-25-320.jpg)









