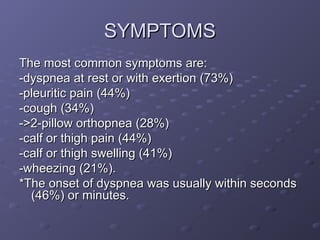
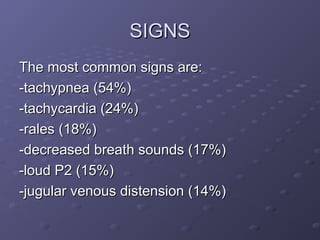
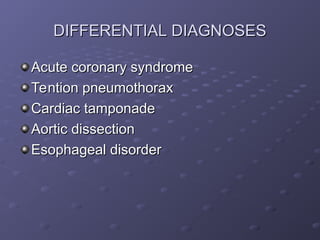
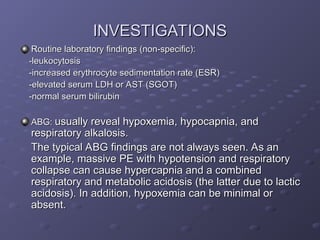
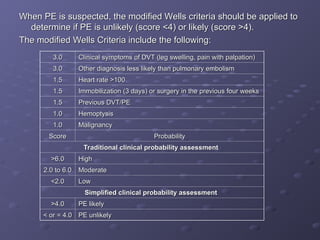
Acute pulmonary embolism (PE) is a serious medical condition with variable and nonspecific symptoms such as dyspnea and pleuritic pain, classified into acute or chronic forms. Diagnosis involves various methods including clinical probability assessments and imaging techniques, while management focuses on supportive care and anticoagulation therapy to reduce mortality. Risk factors include deep vein thrombosis (DVT), recent surgery, and certain chronic conditions, emphasizing the importance of prompt recognition and treatment to improve outcomes.