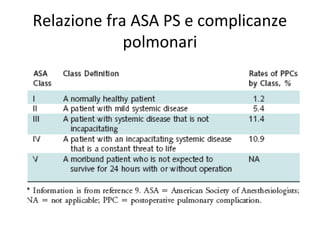
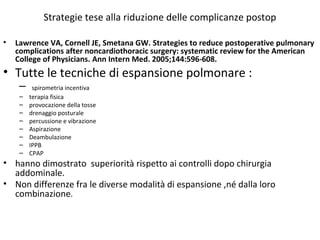
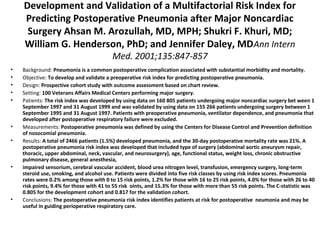
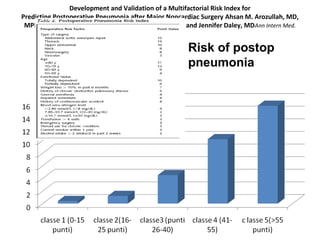
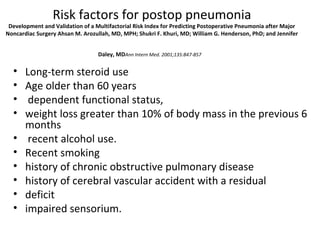
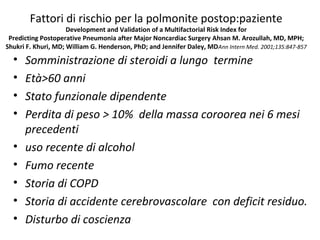
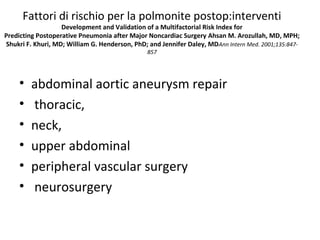
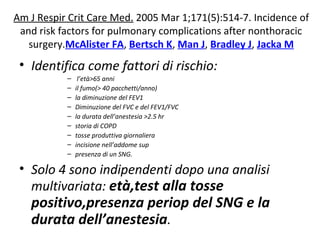
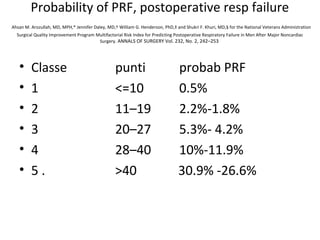
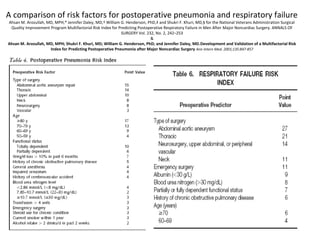
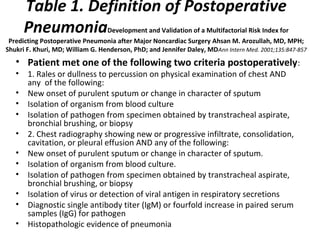
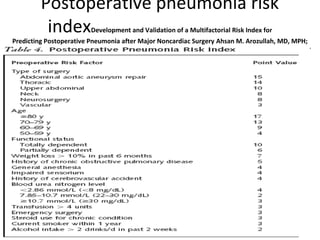
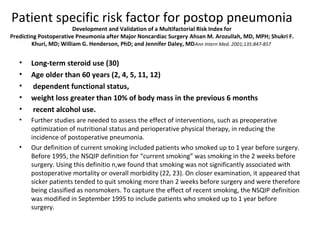
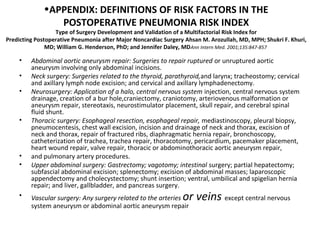
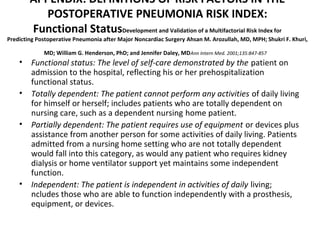
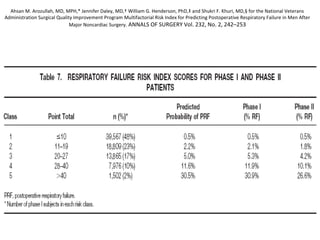
This document discusses the development and validation of a multifactorial risk index to predict the risk of postoperative pneumonia in patients undergoing major noncardiac surgery. It describes defining postoperative pneumonia as new radiographic lung findings accompanied by changes in sputum, a positive blood culture, or isolation of a pathogen from respiratory samples. Risk factors identified for the index included age, functional status, weight loss, COPD, anesthesia type, impaired sensorium, steroid use, smoking, and medical history. The risk index stratified patients into five classes from lowest to highest risk of developing postoperative pneumonia.