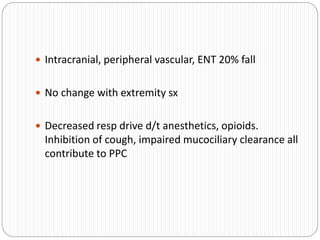
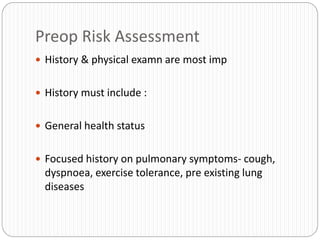
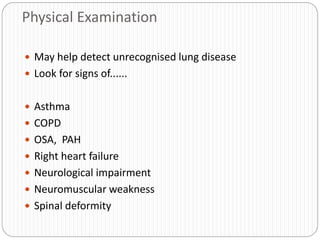
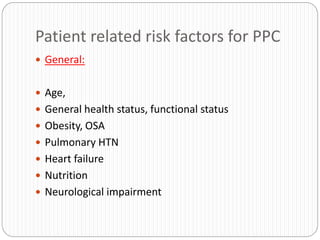
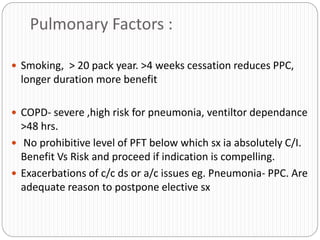
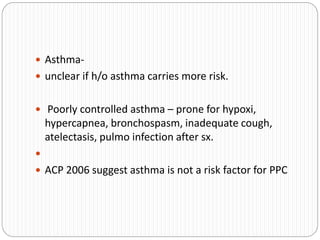
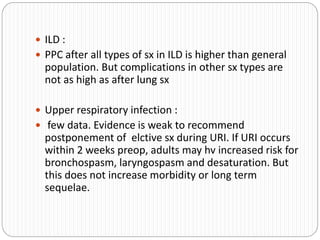
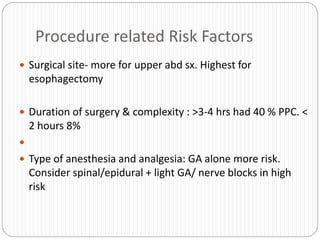
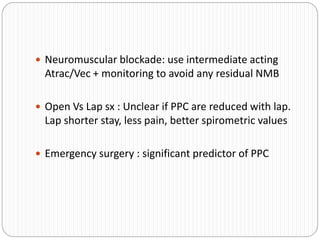
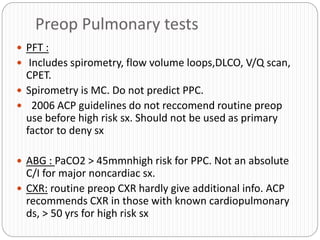
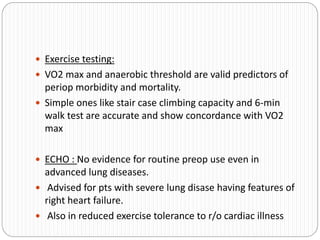
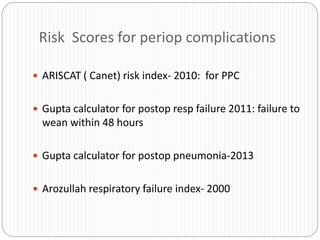
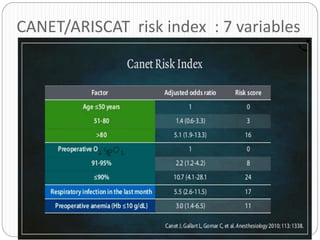
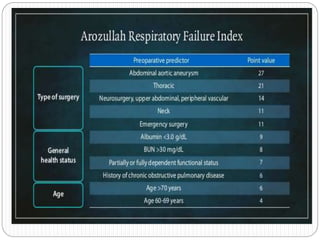
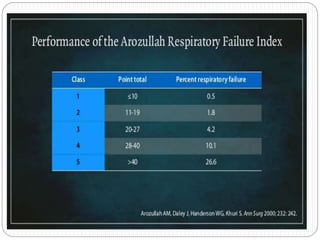
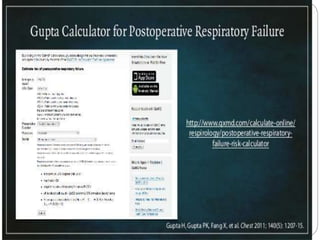
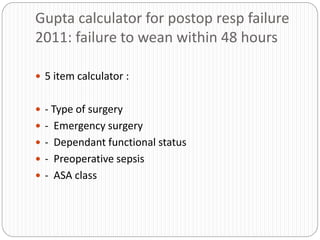
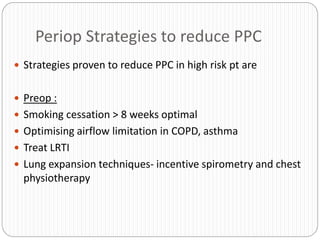
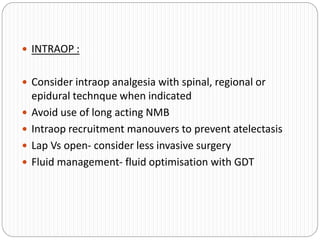
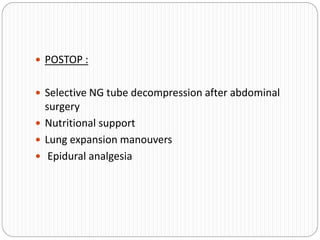
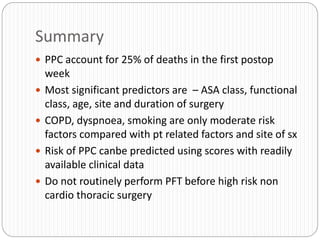
Postoperative pulmonary complications are a major cause of morbidity and mortality after surgery. A thorough preoperative evaluation should identify patient risk factors like age, smoking history, lung disease, and functional status to predict risk. While tests like pulmonary function tests generally do not need to be routinely performed, they may help assess patients with significant lung conditions. Intraoperative and postoperative strategies can help reduce risk of complications in high-risk patients and include lung expansion techniques, appropriate pain management, and fluid optimization. Overall, comprehensive risk assessment allows for optimizing patient health and planning care to minimize pulmonary issues after surgery.