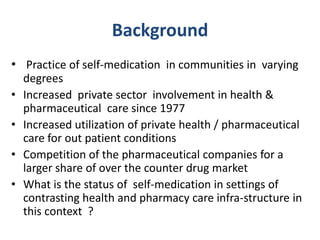
This study examined the practice and predictors of self-medication among adults in both urban and rural areas of Sri Lanka three decades after market economic reforms. The study found that self-medication was more prevalent in urban areas (12.2%) compared to rural areas (7.9%). Conditions of acute onset and short duration were common reasons for self-medication. Predictors of self-medication differed between settings and included factors like household size, drug availability, symptom count, and satisfaction with medical services. The study concluded self-medication is a initial response for less severe diseases based on past experience and recommended its findings be used to shape policy and education programs.