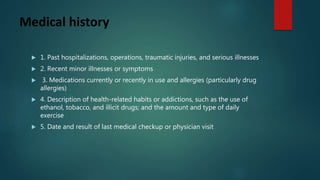
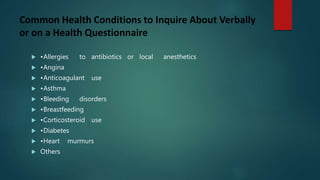
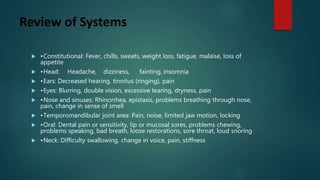
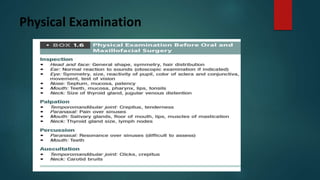
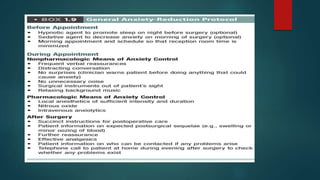
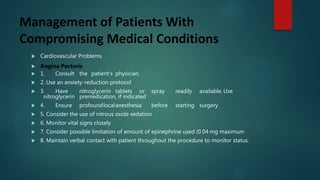
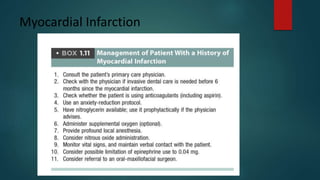
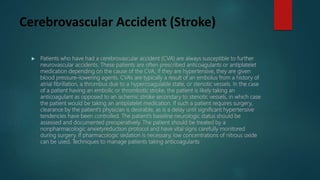
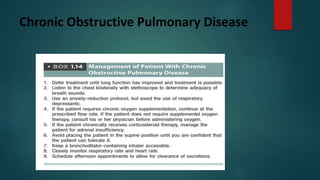
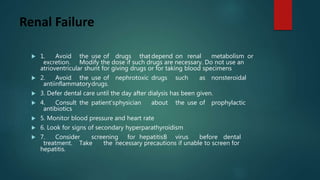
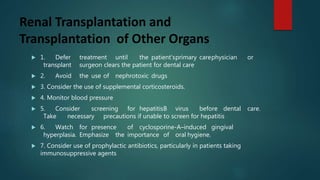
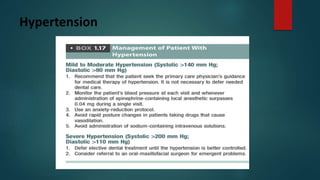
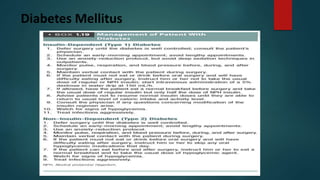
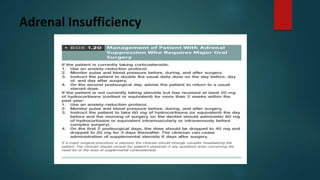
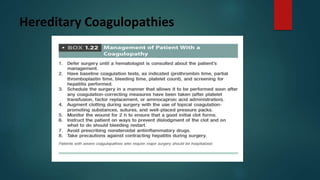
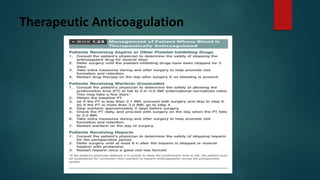
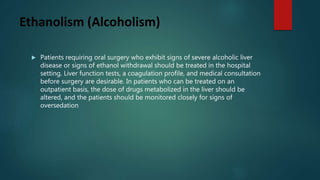
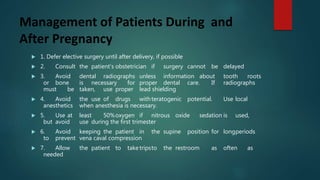
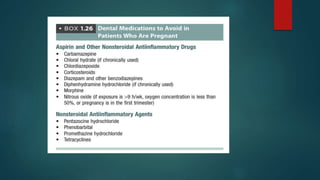
This document provides guidelines for conducting a preoperative health status evaluation. It outlines topics to cover in the patient's medical history including biographic data, chief complaints, past medical issues, medications, and health habits. It also describes a review of systems and physical examination. Common health conditions that should be asked about are listed. The document then provides guidance for managing patients with specific medical conditions such as cardiovascular diseases, pulmonary diseases, diabetes, and pregnancy during dental procedures.