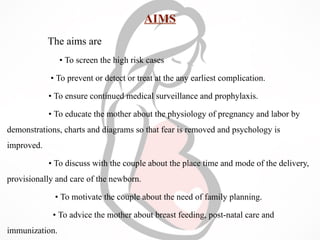
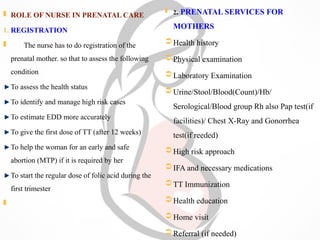
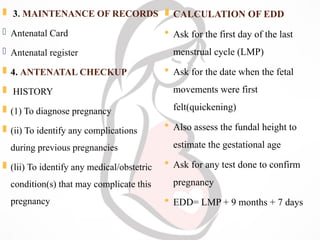
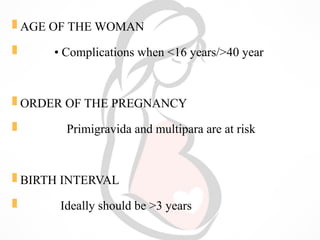
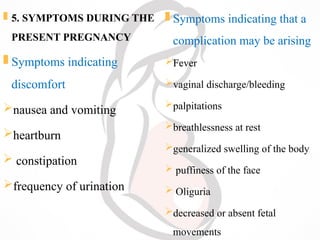
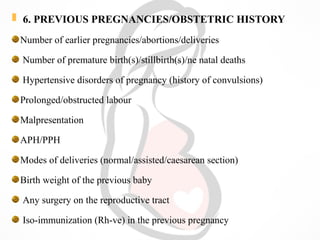
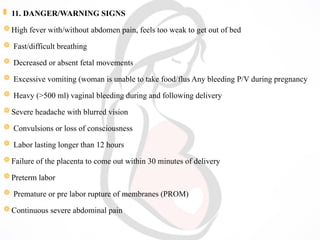
The document outlines prenatal care, which includes regular supervision and advice for pregnant women aimed at ensuring healthy pregnancies and deliveries. It details the roles of nurses in registering mothers, conducting examinations, maintaining records, and providing health education about diet, rest, and the importance of vaccinations. Additionally, the document emphasizes early detection of complications and the provision of antenatal advice to promote the health of both mother and baby.