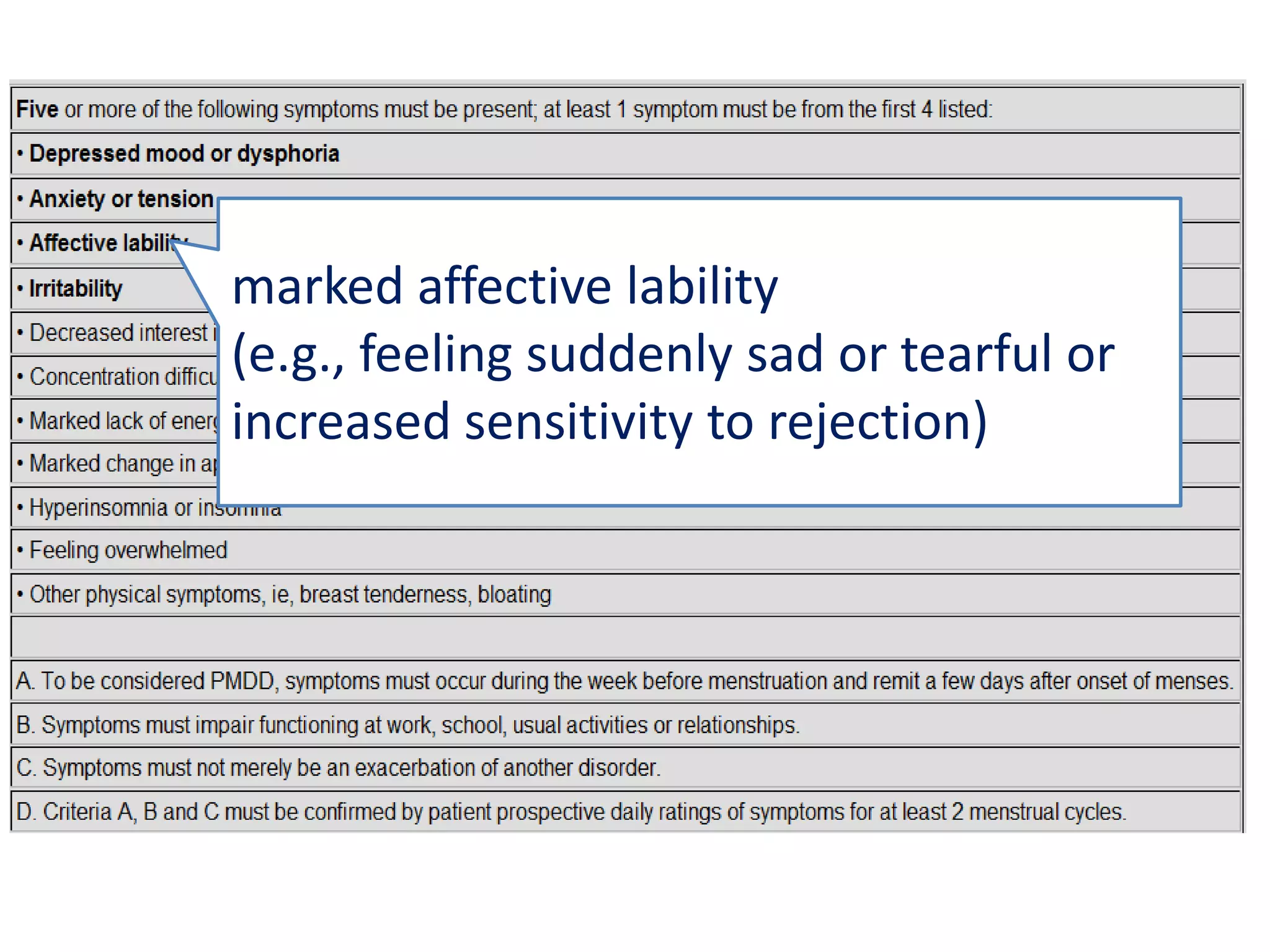
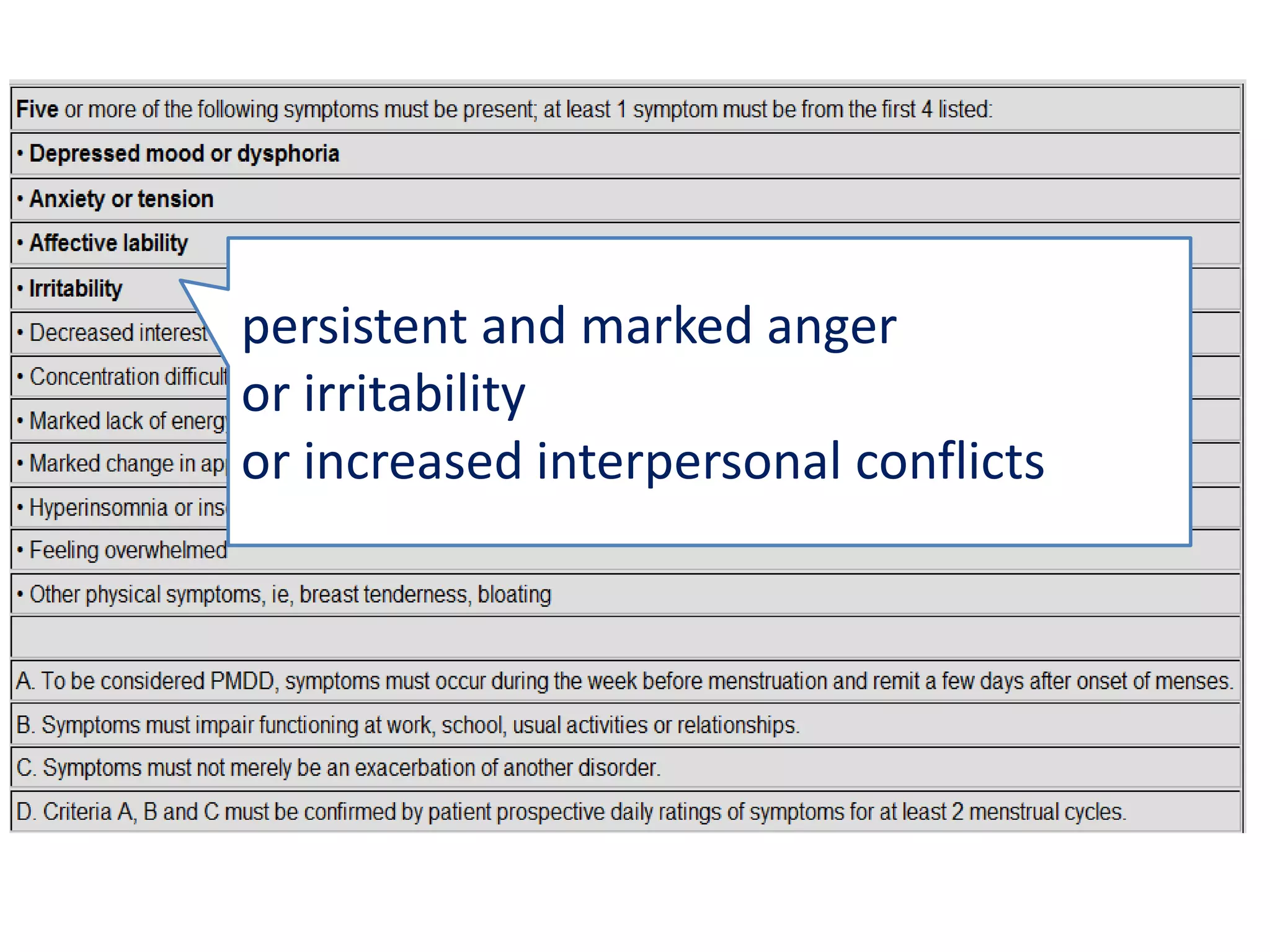
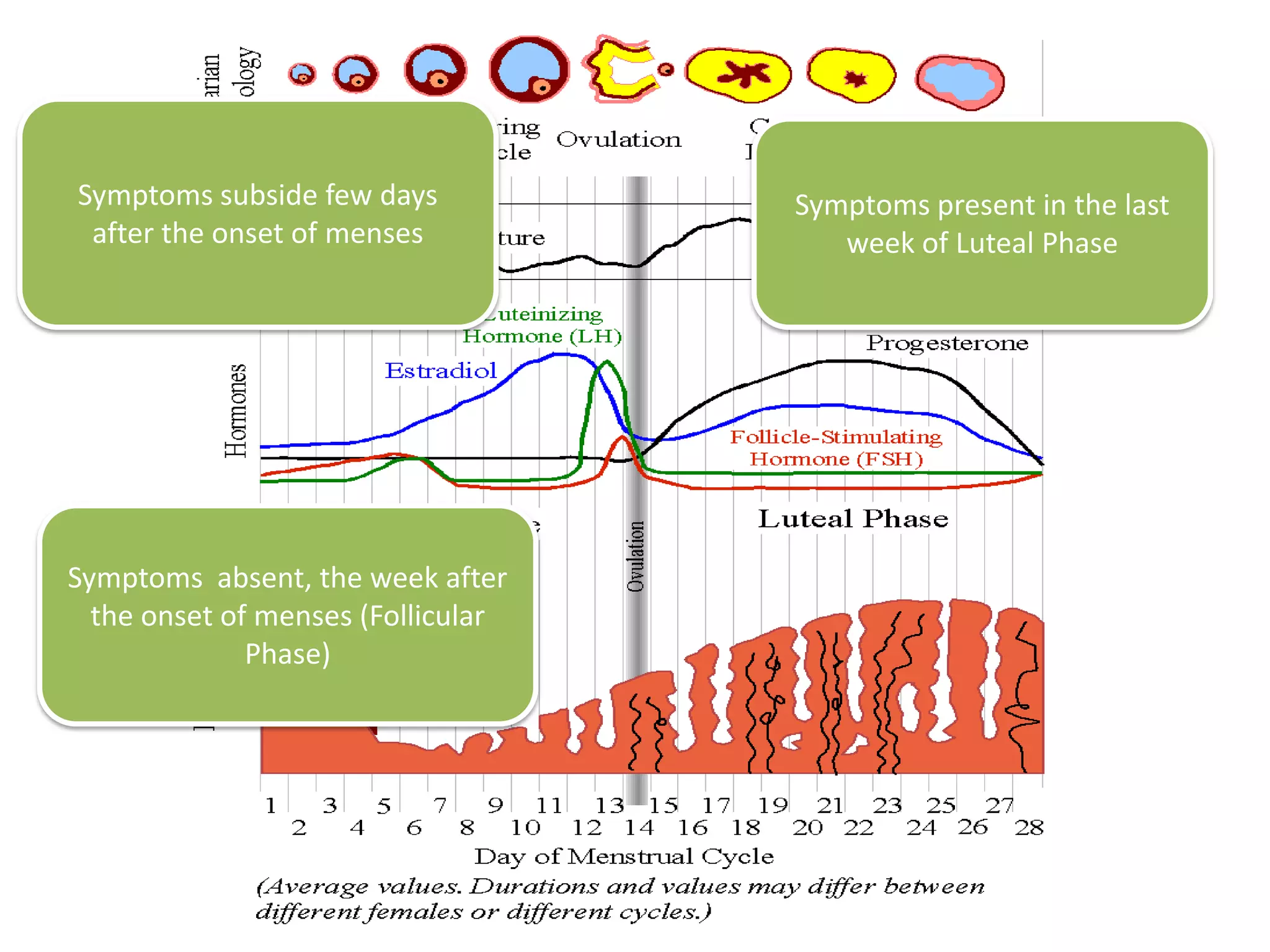
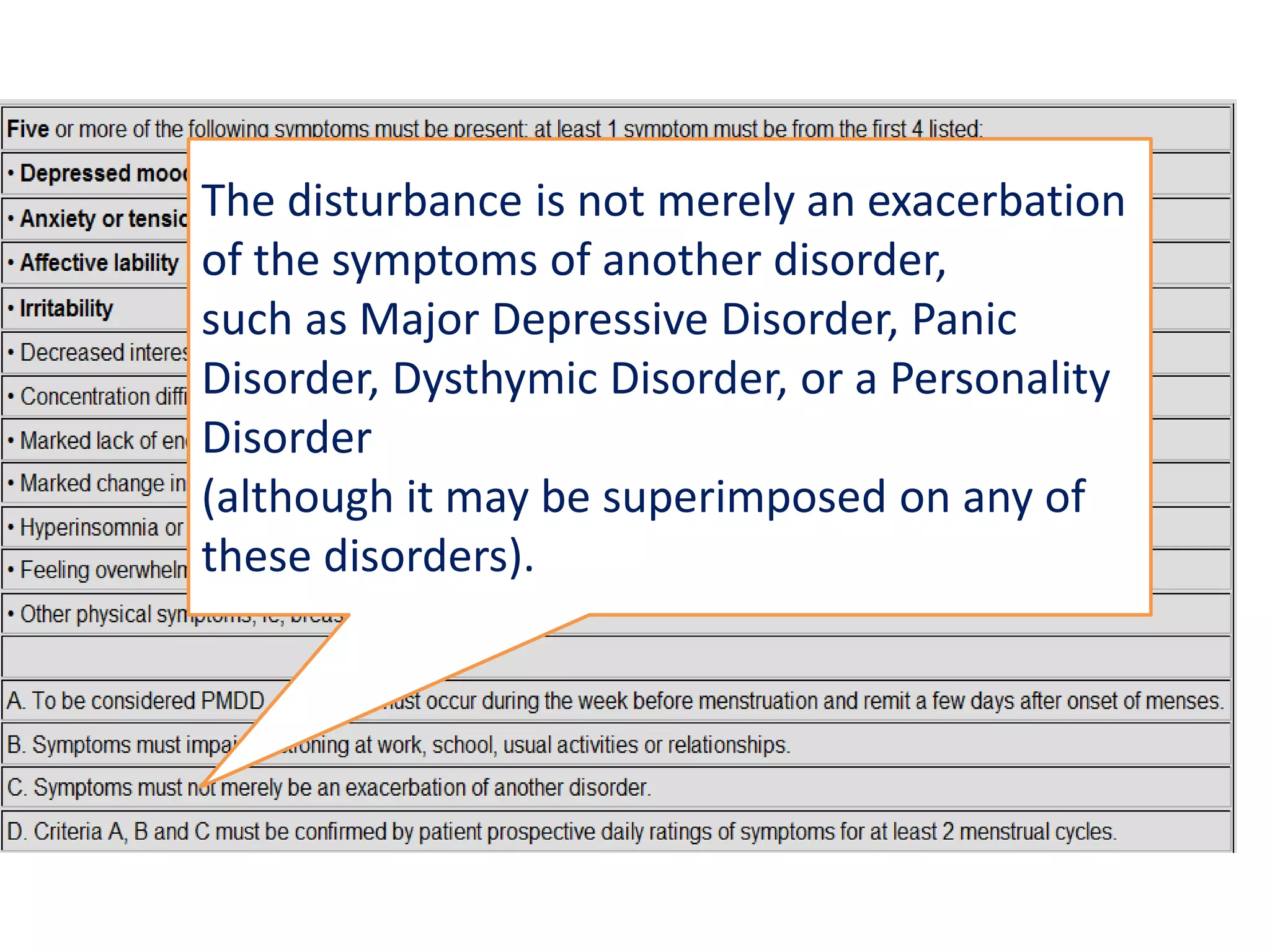
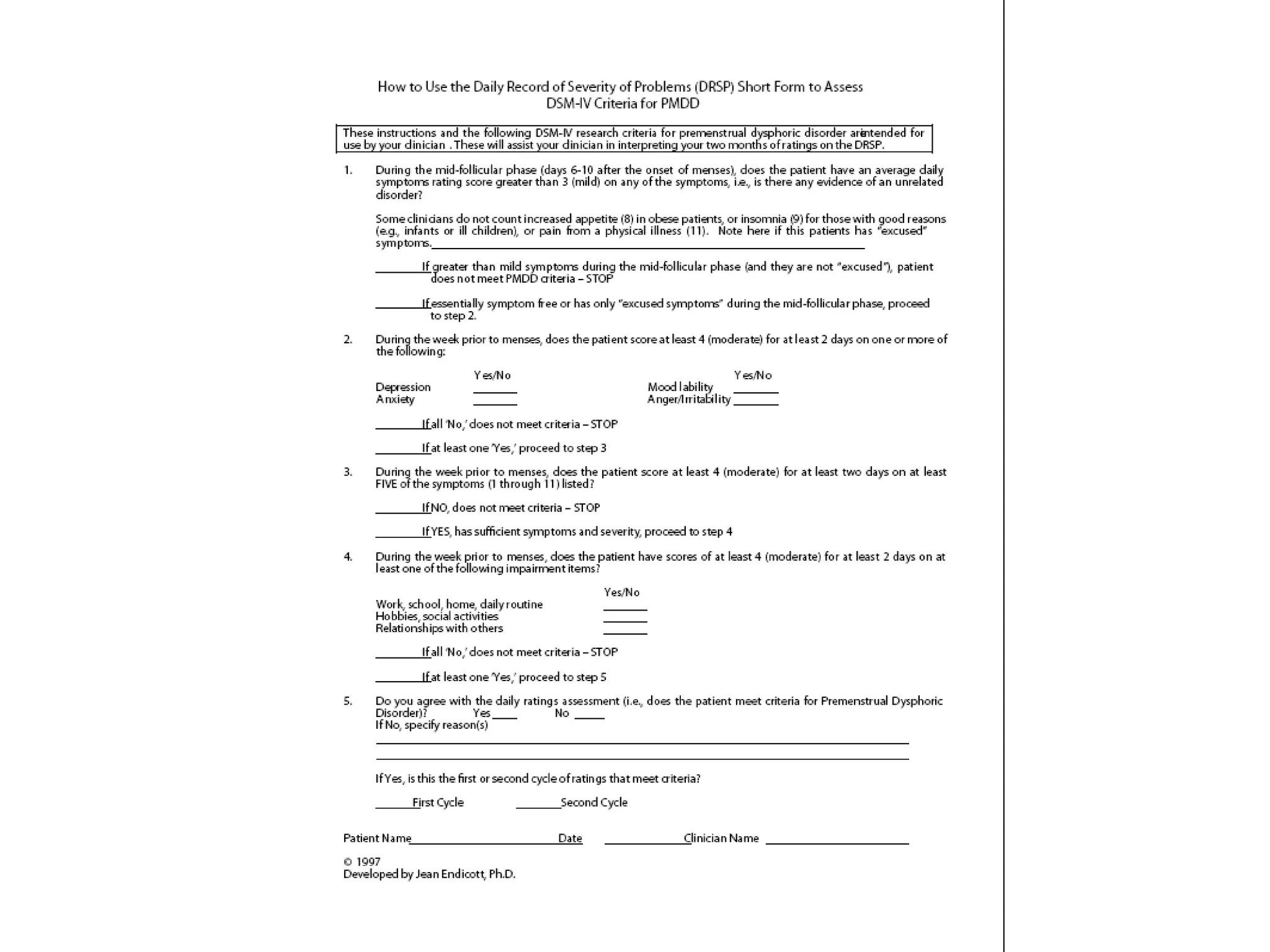
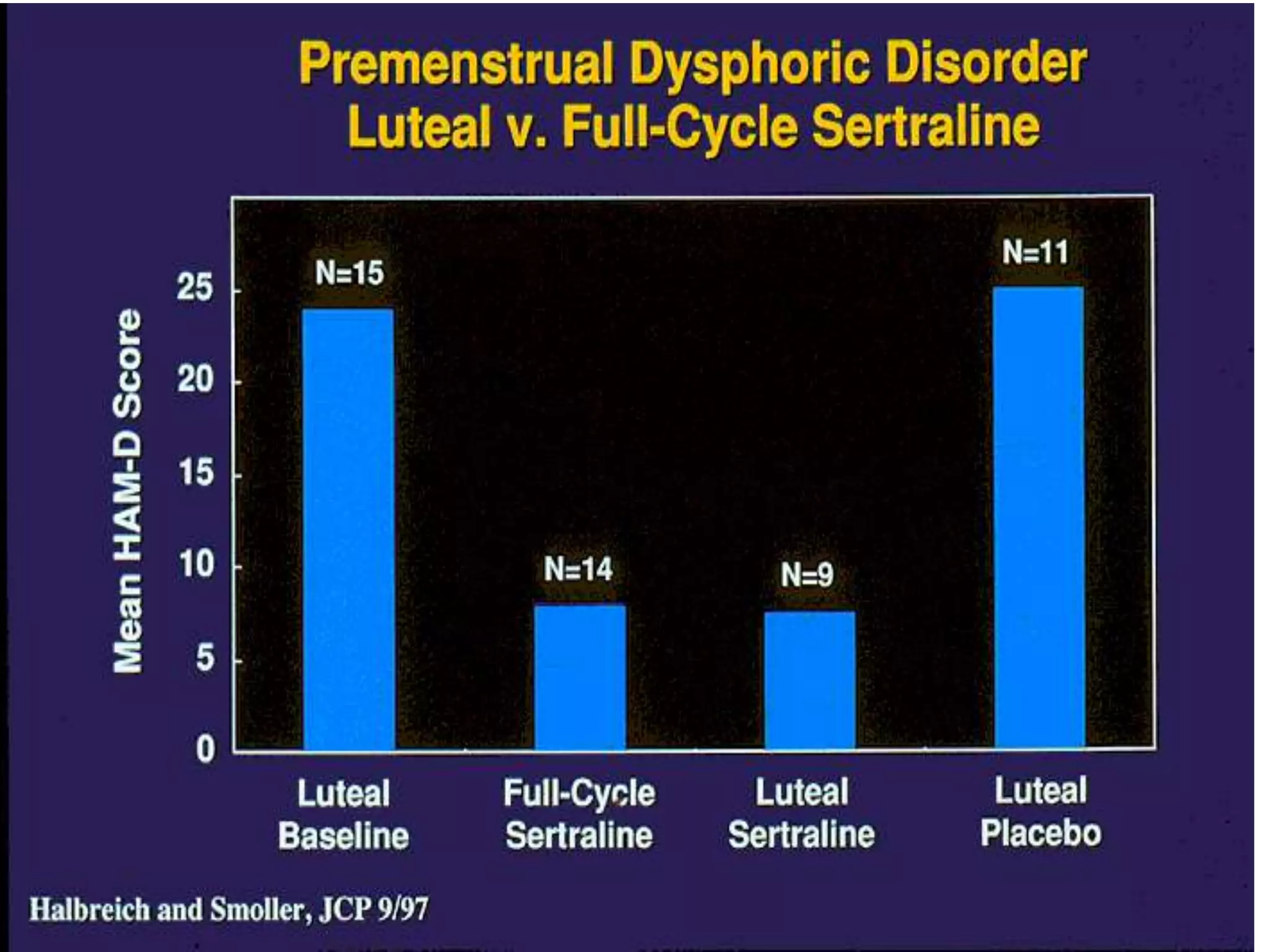
Premenstrual Dysphoric Disorder (PMDD) is a severe form of Premenstrual Syndrome that affects 3-8% of women, causing severe mood changes, anxiety, and impairment in functioning during the luteal phase of the menstrual cycle each month. While the exact causes are unknown, it likely involves an interaction between fluctuating hormone levels and central neurotransmitters like serotonin. Selective Serotonin Reuptake Inhibitors (SSRIs) are effective treatments for PMDD symptoms, suggesting serotonin involvement, though their mechanism of action is complex and not solely due to serotonin reuptake inhibition. PMDD diagnosis requires prospective tracking of symptoms and exclusion of other conditions.