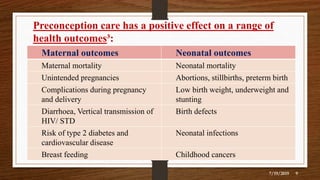
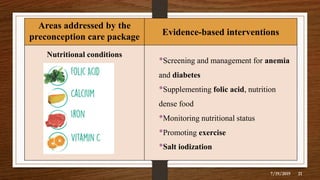
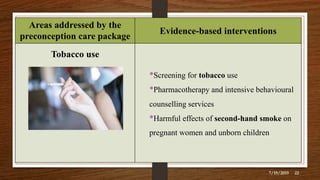
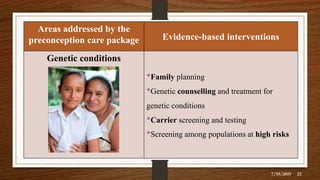
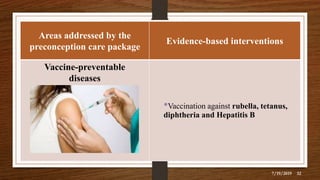
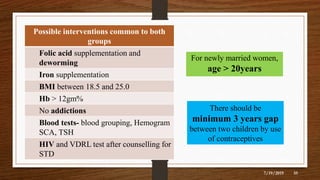
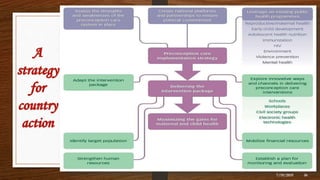
The document presents an overview of preconception care, emphasizing its significance in improving maternal and child health outcomes by addressing various risk factors through evidence-based interventions. Key components include nutrition, tobacco use, genetic conditions, environmental health, and mental health support. It also outlines the importance of national strategies and support from organizations like WHO to achieve maternal and child health goals in alignment with global health targets.