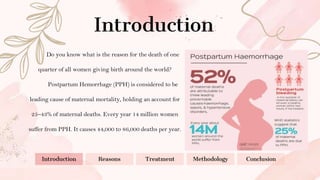
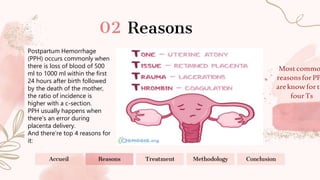
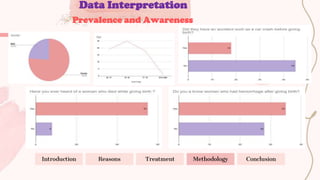
The document summarizes information about postpartum hemorrhage (PPH), which is a leading cause of maternal mortality worldwide. It discusses that PPH occurs when a woman loses 500-1000ml of blood within 24 hours after giving birth. The top four reasons for PPH are uterine atony (weak uterus), uterine trauma, retained placental tissue, and blood clotting conditions. Treatment methods include blood transfusions, uterotonic drugs like oxytocin and misoprostol, and surgery for retained placenta. The document also describes a study conducted to investigate awareness of PPH and its causes and treatments.




![Refrences:
● Evensen, A., Anderson, J. M., & Fontaine, P. (2017). Postpartum Hemorrhage: Prevention and
Treatment. American family physician, 95(7), 442–449.
● World Health Organization. WHO recommendations for the prevention and treatment of
postpartum hemorrhage. Geneva: WHO; 2012. Available from:
https://apps.who.int/iris/bitstream/handle/10665/75411/9789241548502_eng.pdf
● Wormer KC, Jamil RT, Bryant SB. Acute Postpartum Hemorrhage. [Updated 2022 May 8]. In:
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK499988/](https://image.slidesharecdn.com/postpartumhemorrhage-230213192355-5eac5f28/85/Postpartum-hemorrhage-12-320.jpg)
