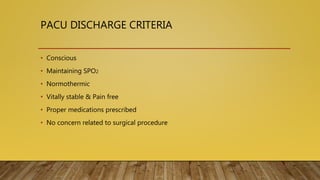
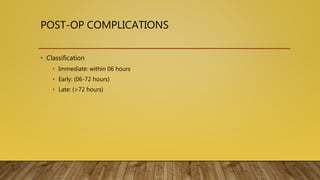
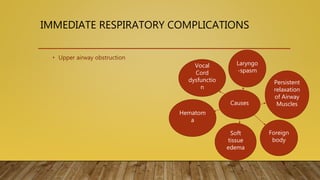
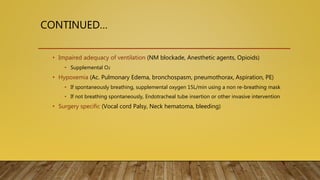
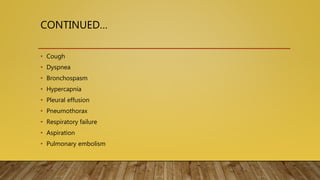
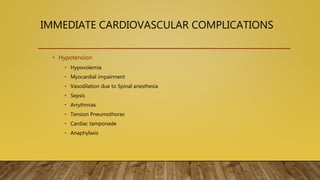
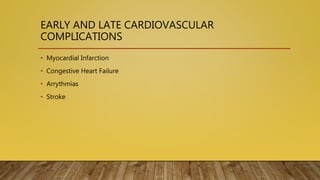
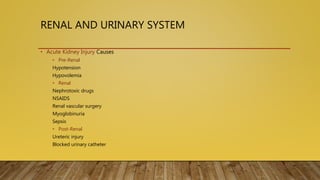
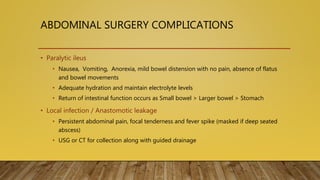
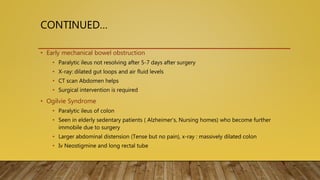
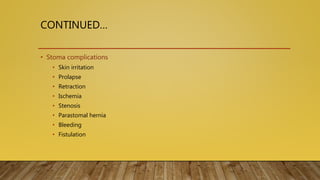
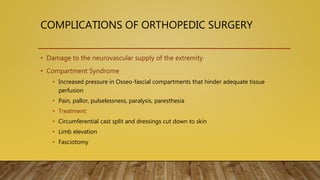
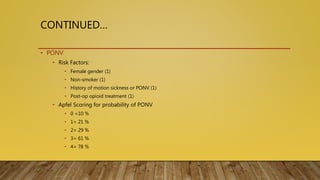
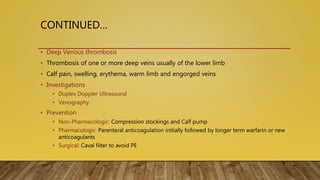
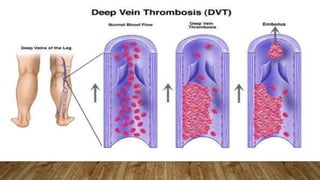
This document provides information on post-operative care, including common complications, their prevention and treatment. It discusses care of patients in the post-anesthesia care unit and criteria for discharge. Some immediate complications discussed are respiratory and cardiovascular issues. Long term complications include infections, DVT and wound healing problems. The importance of early mobilization and physiotherapy to aid recovery is also covered.